Matthew Adinolfi, who has no upper teeth and hasn’t had a love life for over a decade, will be able to get implants so he can kiss a woman without fear of his dentures falling out.
Blanca Coreas, who can’t eat anything firmer than mash without her gums bleeding, will be able to take a bite of roast meat.
Lillian Velazquez now has the root canal she denied for nearly five years.
A class-action lawsuit settled Monday would bring about a change that is as potentially transformative as it is mundane: coverage of common but expensive dental procedures for the five million adults in New York State who use Medicaid, including implants, root canals and replacement dentures.
The lawsuit, filed in 2018 in federal court against the state Department of Health, which oversees Medicaid in New York, accuses the state of denying needed medical care to thousands of low-income New Yorkers.
Medicaid programs, which vary from state to state, are not required to cover dental care. many states do not. But under federal law, if a state Medicaid program covers a optional category of care — such as dental, prescription drugs or optometry — must cover all medically necessary care in that category.
The lawsuit argued that dental health was necessary not only for overall physical health but also for psychological well-being and the ability to find or keep a job.
“You have to have teeth to function in our society,” said Belkis Garcia, a lawyer for the Legal Aid Society, which filed the suit. “It affects everything in your life – your relationships, how people see themselves, how others see you.”
For decades, Ms. Garcia said, New York’s Medicaid coverage rules were “structured to pull your teeth rather than save them.” And because one of the main jobs of a tooth is to hold its neighbors in place, an extraction often has a domino effect: Losing teeth leads to the loss of more teeth.
“Once you start missing a tooth, the teeth start to change,” said Victor Budner, chairman of dentistry at Jacobi Medical Center, an urban hospital in the Bronx. Dr. Badner filed a statement in the case describing the dental needs of one of the plaintiffs.
According to the newly covered benefits, he said, “The vast majority of patients who would otherwise end up losing more teeth may be able to save them.”
New York already had “one of the most generous” Medicaid dental programs in the range of services it covered, said Colin Reusch, policy director for Community Catalyst, a health care consumer advocacy group. But he added: “The devil is in the details in terms of how these policies come into play for people who urgently need special care.”
Under the old rules, root canals and crowns on back teeth were covered only if a diseased tooth was necessary to anchor a denture or if its extraction was medically inappropriate. Replacements for broken or lost dentures were only covered if the dentures were at least eight years old. The implants were not covered at all.
The lead plaintiff in the lawsuit, Frank Ciaramella, died in 2020. In 2018, his dentures were destroyed after he sneezed. they fell out and a car drove them. Under the old limits, he was not eligible for new dentures until 2024.
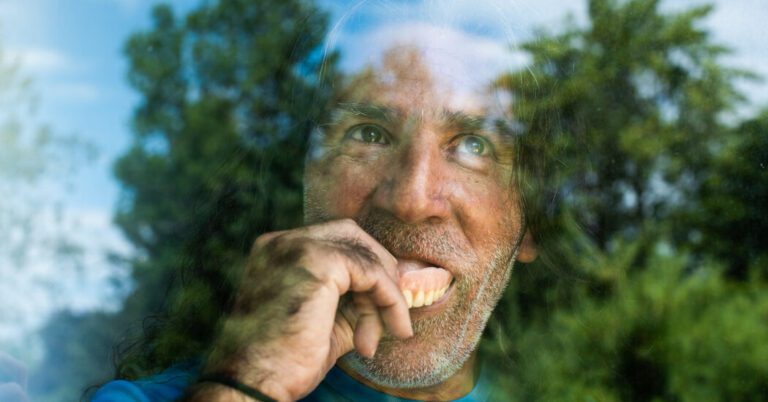
Mr. Adinolfi, 65, a former New York taxi driver who is on disability from a back injury and lives upstate near Plattsburgh, had all but three teeth knocked out around 2010 after contracting an oral infection so seriously the doctors feared that it would spread to his organs.
“It was either pull the teeth or die,” he said.
The dentures he received through Medicaid never fit and wouldn’t stay in place, making it impossible for him to eat with them. He eventually paid for a permanent bridge for his lower front teeth, but couldn’t afford a back one. Years of using his upper gums to chew on his lower dentures left the gums damaged. He needs implants to hold his upper denture in place, but Medicaid didn’t cover them.
As bad as the discomfort and difficulty in eating was, the effect on his social life was at least as bad.
He had not been in a relationship for more than 10 years “because I just get to a point where you want to take it to the next level and then that’s it,” Mr Adinolfi said. “If I take my dentures out, you can see how sucked my face is – it’s just very embarrassing on my part.” (He now has a girlfriend for the first time since his teeth were pulled.)
The settlement obligates New York Medicaid to cover implants, replacement dentures and most root canals if the dentist approves the procedures.
The settlement also removes a rule that barred coverage of multiple procedures for people who still had four matching upper and lower pairs of back teeth, which the state had.considered sufficient for operational purposes.”
Mary Eaton, a solicitor at Freshfields Bruckhaus Deringer, who was involved in the Legal Aid lawsuit, said the teething problems the rules dealt with were “issues everyone faces, regardless of your financial situation”.
But Medicaid recipients tend to have more and more complex health problems than the general population, often as a result lifelong poverty and inadequate medical care. Ms Garcia said she had seen many clients “take on terrible credit card debt” to pay for essential dental procedures.
Gaps in Medicaid dental coverage also exacerbated racial health disparities. Ms. Garcia said black and brown adults suffer from untreated dental disease in almost twice the rate of white adults.
The state Department of Health, which has twice tried to dismiss the case, said in a statement Monday afternoon that the settlement “recognizes the importance of oral health and reaffirms the state’s commitment” to people on Medicaid.
Wesley R. Powell, an attorney with Willkie Farr & Gallagher, which also represented Legal Aid in the lawsuit, said that in the long run, because so many teeth will be saved from being exported, the changes may well save the state money.
Ms. Correa, 62, a former Bronx cafeteria worker, is another plaintiff in the lawsuit. Her dental problems led to digestive problems, vitamin deficiencies, frequent oral bleeding and depression, according to the lawsuit. She said she became socially isolated because people sometimes made fun of her appearance.
In 2019, when Medicaid denied a request for implants, which he needs to effectively wear dentures, he considered suicide. “I felt like I had no support from anyone,” she said.
Ms. Velazquez had an upper molar filled several times, but the filling kept falling out. The dentist told her the tooth needed a root canal and crown, but Medicaid wouldn’t cover it, noting that extracting the tooth would leave her with four matching pairs of back teeth.
For years he avoided eating from the left side to preserve the sensitive tooth. He went through tube after tube of over the counter dental cement. Under an agreement reached before the settlement, Medicaid covered her root canal.
Mr. Adinolfi’s path to dental functionality will be more arduous. He has lost so much bone above his gums that he may need a bone graft from another part of his body or implants anchored to his cheekbone. He faces months of surgeries and long hours in the dentist’s chair.
“I can’t wait,” he said. “I can not wait”.