Volume Restoration
Treatment options
In 2015, hyaluronic acid (HA) fillers made up 80% of all injectable soft tissue fillers, an 8% increase from 2014.11 Hyaluronic acid has achieved enormous popularity as a temporary dermal filler due to its biocompatibility, longevity, and reversibility through hyaluronidase.12
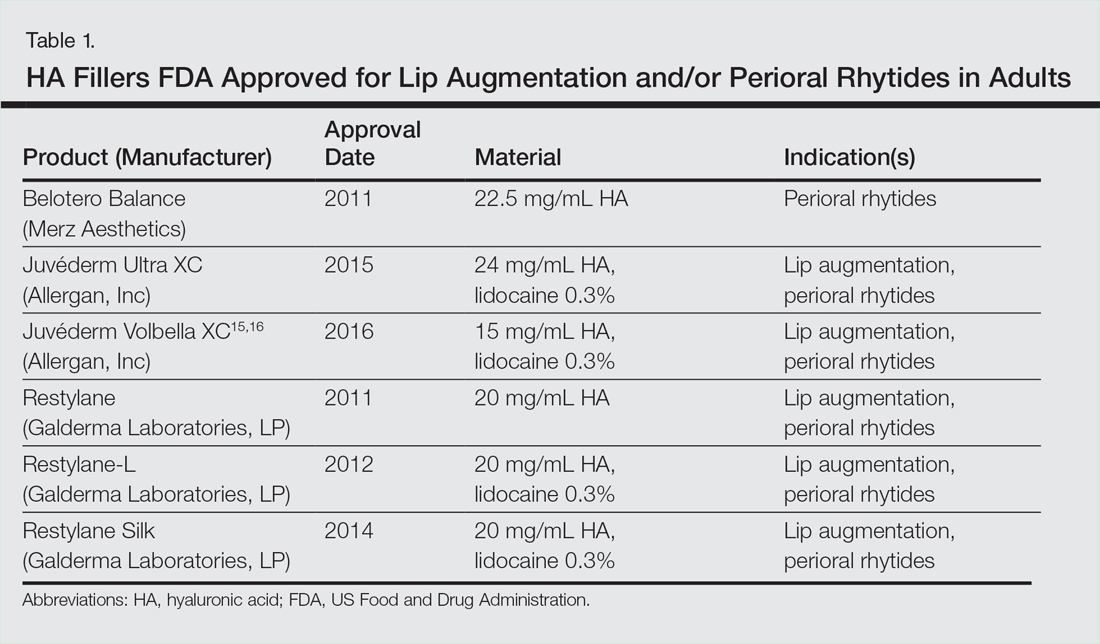
Hyaluronic acid is a natural glycosaminoglycan that comprises the connective tissue matrix. The molecular composition gives HA its hydrophilic property, which increases skin volume.7 Endogenous HA has a short half-life, and chemical modification by a cross-linking process extends longevity by 6 to 12 months. The various HA fillers are distinguished by purification method, particle size, concentration and degree of cross-linking, and viscosity.7,13,14 These differences dictate overall clinical performance such as flow properties, longevity and stability. As a general rule, a high viscosity product is more suitable for deeper growth. Low viscosity fillers are more suitable for correcting shallow defects.1 Table 1 lists HA fillers currently approved by the US Food and Drug Administration for lip augmentation and/or perioral wrinkles in adults 21 years of age and older.15-17
Randomized controlled trials comparing the efficacy, longevity, and tolerability of different HA products are lacking in the literature and, where they exist, are strongly influenced by industry.18,19 The appearance of rating scales provided an objective assessment of perioral and lip augmentation, facilitating comparisons between products in both clinical research and practice.20
Semi-permanent biostimulant dermal fillers such as calcium hydroxylapatite and poly-L-lactic acid are not recommended for lip augmentation due to an increased incidence of submucosal nodule formation.6,14,21 Likewise, permanent fillers are not recommended given the irreversibility and risk of nodules around the lips.14,22 However, liquid silicone (purified polydimethylsiloxane) delivered via a microdroplet technique (0.01 mL of silicone at a time, no more than 1 cc per lip per session) has been used off-label as a permanent filler for lip augmentation with limited complications.23 Regardless, fears about its use in relation to the reported risks still limit its application.22
Similarly, surgical lip implants such as expanded polytetrafluoroethylene are an option for a subset of patients who desire permanent enhancement but are used less frequently given the side effect profile, irreversible nature, and relatively invasive nature of the procedure.22 Finally, autologous fat transfer has been used in the correction of nasolabial and medial folds as well as lip augmentation. However, irregular surface contours and unpredictable longevity due to post-injection absorption (20%–90%) have limited its popularity.3,14,21
HA Injection Technique
Regarding HA fillers in the perioral region, numerous approaches have been described.10.22 The techniques in Table 2 provide the basis for lip rejuvenation.
There are several injection techniques, including serial puncture, linear threading, transverse hatching, and retrograde or anterior fanning.24 A blunt microcannula (diameter 27.38 mm) can be used instead of sharp needles and offers the advantage of increased patient comfort, reduced swelling and ecchymosis, and shortened recovery time.25,26 Gently massaging the product after injection can help with an even contour. Finally, a key determinant of successful results is the use of an adequate volume of HA filler (1–2 mL for vermilion contouring and lip volume).27 Figure 2 highlights a clinical example of HA filler for lip augmentation.
Fortunately, most complications encountered with HA lip augmentation are mild and transient. The most commonly observed side effects include injection site reactions such as pain, erythema and swelling. Likewise, most side effects are related to the injection technique. All HA fillers are prone to the Tyndall effect, a consequence of a very superficial level of injection. Patients with a history of recurrent herpes simplex virus infections should receive prophylactic antiviral therapy.12
Muscle control
An emerging concept of lower face rejuvenation recognizes not only the restoration of volume but also the control of muscle movement. Local injection of botulinum toxin type A induces relaxation of overactive facial muscles through temporary inhibition of neurotransmitter release.6 The possibility of paralysis of the oral cavity may limit the application of botulinum toxin type A in this area.7 However, the off-label potential of botulinum toxin type A has expanded to include several targets on the lower face. The orbicularis oris muscle aims to soften perioral wrinkles. Conservative dosing (1–2 U per lip quadrant or approximately 5 U total) and superficial injection is emphasized in this area.27 Similarly, the oppressive angular muscle is targeted by injecting 4 U bilaterally to soften the marionette lines. In the chin region, the mental muscle can be targeted by injecting 2 U deep into each muscle belly to reduce the mental fold and dimple.28 The combination of dermal filler and neurotoxin therapy demonstrates results that last longer than either method alone and without additional adverse events.29 With combination therapy, guidelines recommend filler therapy first.27
conclusion
A better understanding of the extrinsic and intrinsic factors that contribute to the structural and surface changes of the aging face combined with the preference for minimally invasive procedures has revolutionized the dermatologist’s approach to perioral rejuvenation. Acting as the focal point of the face, the lips and perioral skin are well poised to benefit from this paradigm shift. A multifaceted approach using dermal fillers and neurotoxins may be most appropriate and has demonstrated optimal results in facial aesthetics.