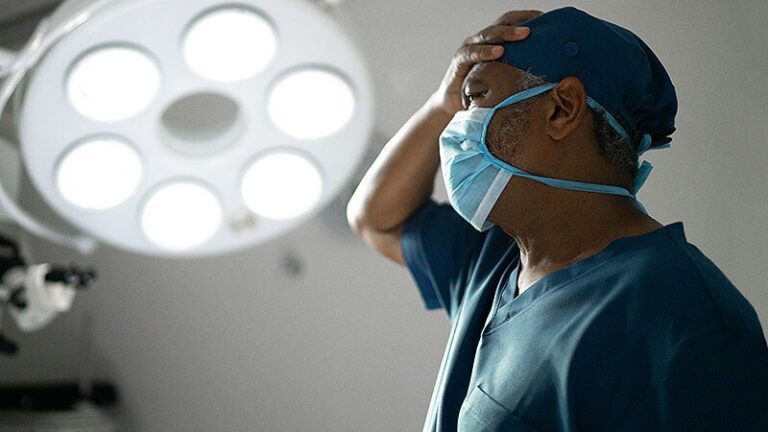
This case illustrates the legal risks that can arise after an adverse surgical outcome.
A 25-year-old woman consulted a plastic surgeon for a breast lift. She weighed 157 kg and her breast size was 37D. The surgeon recommended a breast lift with implants. The patient signed a seven-page consent form that described specific risks, including tissue necrosis. She was given antibiotics before mastopexy and augmentation.
During the 7-hour surgery, the surgeon removed 327g of tissue from the left breast and 414g from the right. Photographs taken postoperatively showed pink nipples. Antibiotics were administered after surgery.
At the office visit 1 week after surgery, cultures were negative but levofloxacin (Levaquin) was prescribed again. During the second office visit 2 days later, the surgeon applied a cross dressing to the chest area because of the swelling. Four days later, an external ultrasound was used to assess the cause of the swelling. It was noted that the loops were changing color. The surgeon asked the patient to return to the office in 2 days.
At the next office visit, the surgeon noted clear drainage. Examination of both breasts revealed blisters and erythema around the incision sites. The blisters were removed. civilizations grew Alcaligenes, and the patient was referred to an infectious disease specialist. He noted bilateral necrosis in areas around the nipples, with vertical incisional inflammation consistent with infection. Start the patient on IV antibiotics.
Two weeks later, the infectious disease specialist noticed indurated black eschar (a dry, dark crust) involving both nipple areas, with some wound breakdown and underlying fat necrosis. Ten days later, wound cultures were positive for Pseudomonas aeruginosa. The patient was started on Levaquin and referred to a wound care specialist who started hyperbaric treatments.
The patient underwent several stages of reconstructive surgery. She now has severe scarring and disfigurement of both breasts. A lawsuit was filed against the plastic surgeon.
Expert reviewers were critical that too much breast tissue had been removed and that the implants compromised the patient’s circulation. The case was eventually settled.
While it could be debated whether the surgeon removed too much breast tissue or made a mistake elsewhere in the procedure, the fact is that surgical results are not good. To reduce your legal risk, it is beneficial for doctors to help patients set reasonable expectations about outcomes before procedures. Additionally, discuss with patients the potential for less than optimal outcomes and complications that could delay recovery and affect appearance.
An informed patient often has more realistic expectations and may be more understanding if outcomes change for the worse.
This case is from The Doctors Company claims database. For more case studies on this topic, seePlastic Surgery Closed Claims Study.”
Communication monitoring gives rise to a legal claim
Even if you take all the right steps during a procedure, a physician’s duty may be inadequate if all necessary information is not communicated to a patient. This case demonstrates why the informed consent process is so necessary and how easily a miscommunication can cause an unfortunate legal outcome. A female patient in her late sixties presented to a pain management physician with pain in her neck and low back. She was treated with multiple cervical steroid injections and epidural steroid injections in the lumbar spine.
A few days after a recommended medial branch nerve block, the pain management physician performed a radiofrequency ablation of a medial branch nerve. He had another removal 2 weeks later. At a follow-up appointment, he reported that the pain had decreased by 50%.
Two months later, the patient reported continued pain in the lumbar region. The pain management doctor recommended a trial implantation of a spinal cord stimulator electrode, a device that can relieve pain through low levels of electrical energy sent directly to the spinal cord. The patient agreed and had excellent coverage during the neuromodulation trial. The recommendation was to proceed with the permanent implant.
The pain management physician reviewed the procedure with the patient. Leads were placed, under fluoroscopy, at the superior portions of C2 and C3, with anchor sleeves slipped over the leads and connected with sutures.
Two months after the procedure, the patient returned to the pain management physician’s office complaining of a headache and some low back pain. This pain persisted and the patient sought a neurology consultation. The impression was spinal cord stimulator migration, occipital neuralgia and degenerative disease of the cervix.
The headaches continued. The pain management doctor did a series of occipital nerve blocks. Five months after the permanent stimulator implantation procedure, another provider removed a scalp mass that was discovered to be an anchor from the stimulator wires. The patient filed a claim against the pain management physician.
What did the experts say?
The expert medical commentators noted that it was not under the standard of care to leave the anchor in after the implant. However, it was below the standard of care not to inform the patient that anchors were left in place. Additionally, an expert medical reviewer opined that the pain the patient was experiencing was not from the anchor but was related to occipital neuralgia. Lack of communication about the anchor led to a small settlement.
Although the physician was not negligent in implanting the spinal cord stimulator, this case allowed for a lack of communication with the patient regarding the remaining anchors. The scenario highlights the importance of having a robust informed consent process. Physicians should ensure that patients fully understand all important elements of a procedure and ask patients to repeat information to ensure understanding.
Informed consent does not completely eliminate liability claims, of course, but a solid doctor-patient relationship based on comprehensive information exchanges can help reduce patient frustration about an outcome and reduce the risk of claims.
This case comes from “Pain Management Closed Claims Study”, published by The Doctors company.