People who are more susceptible to a serious heart infection could be at risk of dying from the condition by not taking antibiotics at the dentist, according to researchers.
Prescribing antibiotics to patients at higher risk of developing infective endocarditis (IE) – an inflammation of the inner lining of the heart – before dental work can save lives and save the NHS money, they claim.
The National Institute for Health and Care Excellence (Nice) recommended against antibiotic prophylaxis, or when antibiotics are given as a precautionary measure to prevent infection, for those at risk of IE undergoing dental procedures in 2008.
Researchers are now calling on the NHS spending watchdog to review its guidelines.
But Nice rejected the claim that patients were being harmed and said that while using antibiotics in this way is not routinely recommended, healthcare professionals “should use their clinical judgement”.
It is understood that around 400,000 people in the UK are at high risk of IE whenever they have dental work, with an estimated 261 people a year contracting the infection and 78 dying from it.
According to the NHS, it is more common in older people, although it has been detected in children born with congenital heart disease.
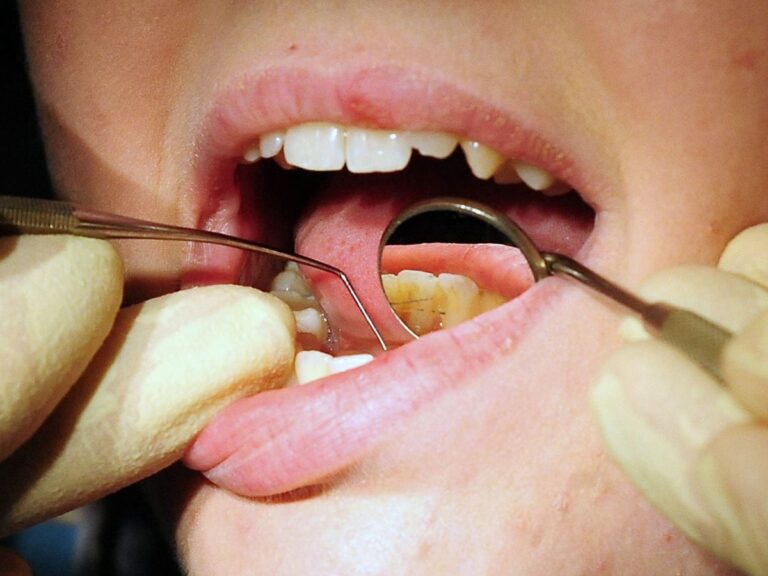
About 30% to 40% of cases are caused by bacteria from the mouth, either from poor dental hygiene or invasive dental treatment such as tooth extraction.
A study led by the University of Sheffield’s School of Clinical Dentistry claims the risk of IE is one in 1,000 among high-risk patients undergoing dental work as a whole.
However, the odds are revised to one in 3,333 if antibiotics are given before treatment.
The findings – published in The Lancet Regional Health – also suggest that the risk among those having tooth extractions is one in 100 in the absence of antibiotic prophylaxis, which drops to one in 1,000 when antibiotics are used.
In high-risk patients undergoing oral surgery, the risk of IE is one in 40, falling to one in 500 with antibiotic prophylaxis.
Lead author Professor Martin Thornhill, of the University of Sheffield’s School of Clinical Dentistry, said: ‘Infective endocarditis is a rare but devastating heart infection in which around 30% of people die within the first year of its onset.
“All major guideline committees worldwide, such as the American Heart Association and the European Society for Cardiology, recommend that those at high risk of infective endocarditis should receive antibiotic prophylaxis before undergoing invasive dental procedures.
“We urge Nice to review its guidance so that high-risk patients in the UK receive the same protection against IE as patients in the rest of the world.”
A Nice spokesman said the watchdog “rejects the claim that patients are being harmed as a result of our guidelines”.
“The guideline says that antibiotic prophylaxis against infective endocarditis is not routinely recommended in people undergoing dental procedures,” they add.
“However, healthcare professionals should use their clinical judgment when implementing recommendations, taking into account the individual’s circumstances, needs and preferences.
“Our surveillance team is going to review the current evidence on infective endocarditis prophylaxis this year and determine whether any new information, studies or research will support the case for further updating the existing Nice guidelines.”
Prof Thornhill claims that preventing between 40 and 260 cases of IE a year could save the NHS more than £5.5 million.
“There are currently 400,000 people at high risk of developing IE in the UK and this number is increasing every year due to the increasing number of patients having cardiac procedures,” he said.
“Our previous study showed that prescribing antibiotic prophylaxis would be cost-effective if it prevented just 1.4 high-risk patients per year from developing infective endocarditis.
“Thus, by preventing between 40 and 260 cases per year, antibiotic prophylaxis would be highly cost-effective and likely to save the NHS over £5.5m per year, as well as creating significant health benefits for those at risk of endocarditis ».
Mick Armstrong, chairman of the British Dental Association’s Health and Science Committee, said “dentists are taking a responsible approach to antibiotics”.
“Some fellow doctors want us to be more generous with prescriptions,” he added.
“Yes, a small number of vulnerable patients may benefit, but we must focus on keeping these vital medicines for everyone.
“When practices became closed during the lockdown, the government encouraged a free antibiotic for all in dentistry. Antibiotics do not cure a toothache. And they are no substitute for timely access to routine and emergency care.
“Antimicrobial resistance represents an existential threat to modern healthcare. Clinicians must carefully balance risks and benefits. And the Government must go much further to ensure that NHS dentistry even has a future.”