This paid piece is sponsored by Siouxland Oral & Maxillofacial Surgery.
We’re back to talking about dental implants again, but this time let’s focus on some of the supportive procedures that need to be done before an implant is placed. Some cases are just perfect: plenty of bone, the right space, and enough of what we call attached gum. Many cases, however, are not perfect and therefore need a little help to get them where they need to be.
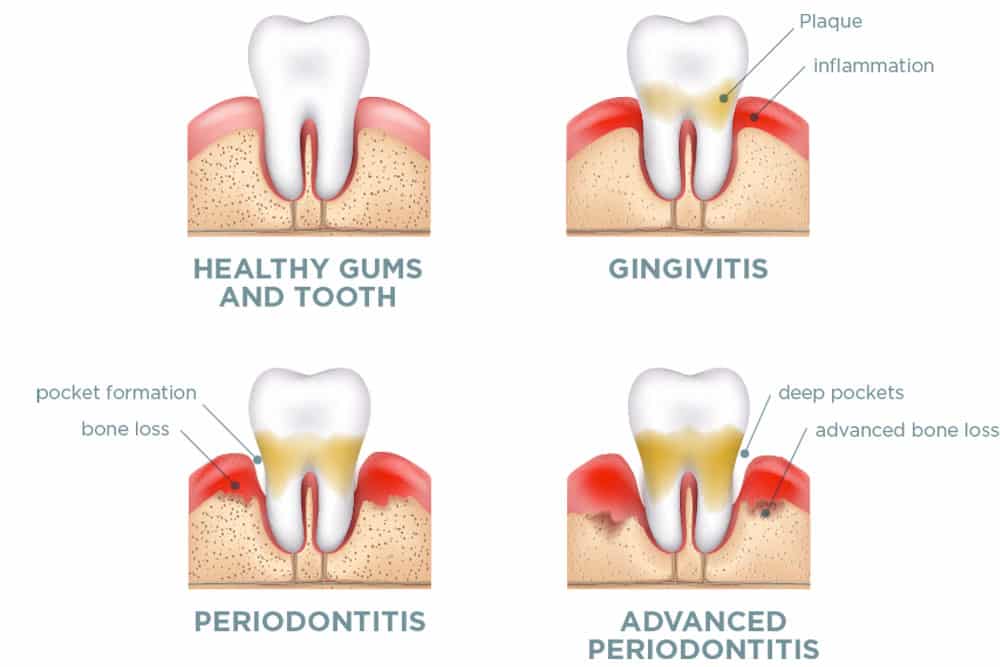
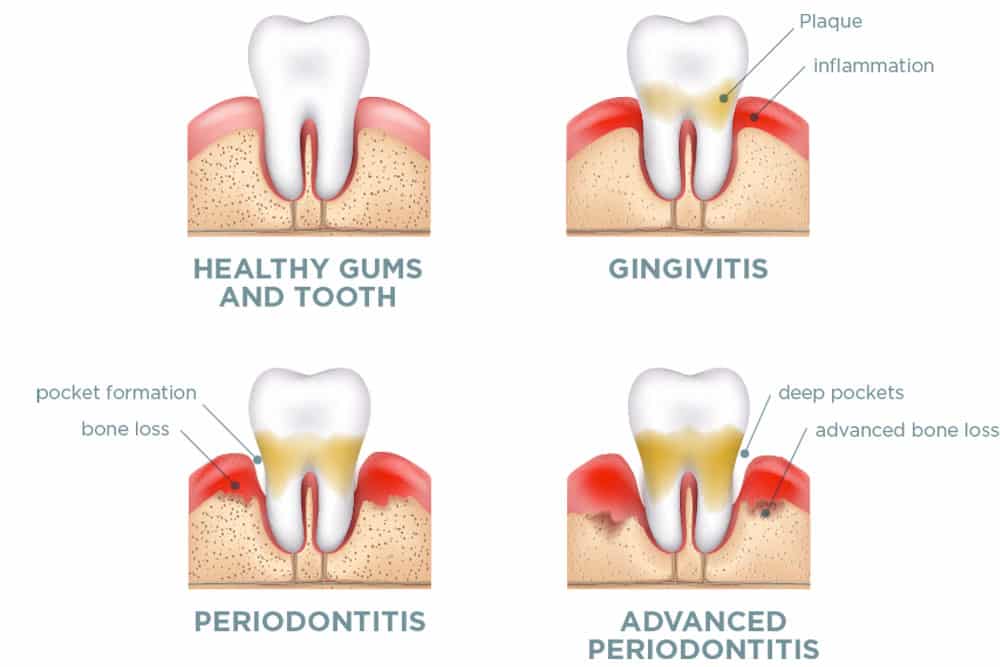
One of the most important things to manage is the amount of bone you have in order to have a successful dental implant placement with longevity. There are many ways that people can lose bone, but they may not even realize it. Bone loss can be caused by periodontal or gum infections, disease or even trauma and other types of tooth infections. Many other people lose bone because of the inflammatory effects of infection around decayed or broken teeth. This can be vertical bone loss or loss to the buccal, or cheek, side of the tooth.
This buccal plate, as we call it, is critical to establishing the correct placement of the dental implant. If it is not there, it makes the job of placing the implant difficult. Sometimes, the extraction of a tooth can completely break the bone in the mouth. this is more common for teeth with multiple roots. So we almost always cut multi-rooted teeth, such as your molars and premolars, into multiple pieces so that there is less risk of fracturing the oral plate.
For example, let’s say you had a tooth extracted and everything went well. More and more often, we can place an implant at the same time as the extraction of the tooth, with the idea here that the dental implant will occupy most of the extraction area and will be anchored a few millimeters after the extraction point in fresh bone. However, this is not always possible because you may end up in the maxillary sinus or encounter a nerve that provides sensation to the lower lip. In these cases, it is best to wait for the body to regenerate the bone and gum tissue in that area. The patient can then return four to six months later to have the implant placed.
Some extraction sites require bone grafting to maintain the architecture or form of the bone where the implant will go. However, not every area needs bone grafting. There are times when the implant will need to be placed a little lower at the extraction site that still has good cortical walls. Before agreeing to a bone graft, you need to know and understand the rationale and anatomy behind it.




Many times, when you immediately place implants right after tooth extraction, there is a gap between the implant and the walls of the extraction site. If the gap is greater than 1 millimeter, you will definitely need a bone graft to act as a road map for the body to know to build bone in the area and stick to the implant.
So you may be wondering how to decide when it’s a good time to go back if you don’t get an implant right away. Generally, it’s six months, but ideally, you’d go back and have a CT scan to see if the outer covering of the bone, called the cortical bone, has actually reformed. If it has, then the area is ready for implantation.
When you place a direct implant to replace a back tooth, sometimes you need to make small casings at the attached position and angle to make the implant really stable. With custom crown attachments to be placed later, this will make very little difference to the look and feel of the new ‘tooth’. However, there will be some criticism of the position and angles on the radiographs. Waiting for the area to fully heal is the ideal option. However, for various reasons, many people still want immediate implants.
For single-rooted teeth in the front of the mouth, direct implants are a simpler procedure with more chances for correct angles and positions. An advantage of immediate implant placement for anterior teeth is that they tend to preserve oral bone and soft tissue architecture for better cosmetics.
Newer implants with different placement drills, thread designs, and connections allow greater osseointegration than previous designs. The newest implant shows a connection of up to 50 percent to the bone compared to the previous design that weighs only 30 percent. This creates better force distribution throughout the length of the implant and does not concentrate forces on the neck of the implant as it exits the bone. In addition, the new prosthetic connection of three oval teeth allows for more thickness and stability of the oral bone.
These are just some of the things we think about and can talk about when we have a pre-extraction consultation or discussion about direct implants. Combine this with our previous articles on different implant materials, such as ceramic implants, and you’ll see that you have many options to ask your oral surgeon. There are more and more people trying to get implants, so as you choose where to have your procedures done, make sure they have all the tools and knowledge to offer all the different options available.
Thanks for reading it! See you next month, friends.






