Preoperative assessment
Implicit understanding of the patient’s concerns is a necessary condition for the planning and technical execution of any operation. Once the patient and surgeon have a mutual understanding, a comprehensive plan can be constructed that incorporates the patient’s wishes, their underlying anatomical issues, the surgeon’s observations of the problem, and the limitations of the procedure. The consultation should first focus on the patient’s global medical and surgical history, eliciting any issues that may preclude or increase the morbidity of the surgical plan. Chronic medical conditions such as heart disease, hypertension, diabetes mellitus, liver disease, thyroid disease, and bleeding disorders should be induced. A more focused surgical and medical history should be obtained, focusing on previous eye surgery such as photorefractive keratectomy and underlying ophthalmic conditions such as blepharochalasia.
Following the patient’s history, a comprehensive review of systems should be performed, specifically asking the patient about excessive lacrimation, dryness, frequent blinking, redness and burning of the eyes, and contact lens wear.
Of the aforementioned symptoms, dry eyes deserve special attention. It can have multiple causes, including insufficient tear production and excessive tear evaporation. Complaints may include itchy eyes, foreign body sensation, blurred vision, pain, and eye fatigue. In the general population, 12% of men and 17% of women experience dry eye symptoms.
[30] If one suspects that a patient may have dry eye syndrome or other eye complaints, referral to an ophthalmologist is appropriate.
There are many risk factors for dry eye, including environmental, pharmacologic, and systemic disease, however it is important as a surgeon to identify anatomic risk factors during physical examination and then plan accordingly. A history of previous eye surgery such as LASIK, cataract surgery, or even previous blepharoplasty also increases the risk of dry eye.
[31] In summary, the Schirmer test has not been shown to be a reliable predictor of patients at risk for dry eye, but rather a detailed history and focused physical examination is a more useful tool.
[32]
Chronic allergies, tobacco use, alcohol use, and current medications, including herbal supplements, should also be noted. In particular, aspirin and the use of other anticoagulants should be documented. The underlying condition that requires the use of these drugs must also be determined and a decision made if discontinuing these drugs is safe for the patient. Bleeding complications can lead to severe morbidity that is exacerbated by the fact that blepharoplasty is an elective surgery. It is our practice to discontinue the patient’s aspirin and antiplatelet agents two weeks prior to surgery and for one week after, if the patient’s medical condition allows such discontinuation.
Natural
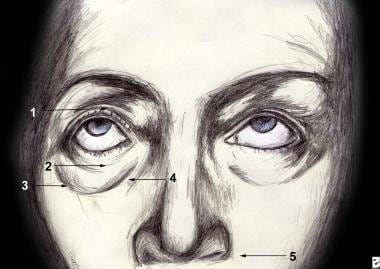
The physical examination should document the anatomic structures that make up the lower eyelid as well as the surrounding periorbital architecture as it relates to the patient’s concerns. Carefully note the superficial anatomy of the periorbital region (see image below). This investigation should also note any anatomic variations that may predispose to postoperative morbidity.
Topographical anatomy of the eyelid. 1.Superior tarsal fold 2.Inferior tarsal fold 3.Valpibromidal groove 4.Rhinoscopic groove 5.Nasolabial fold. Adapted from Jelks, 1993.
In order to devise a comprehensive surgical plan to address the patient’s concerns, the surgeon must have a keen understanding of facial and periorbital aging. The youthful face is strongly characterized by elastic skin without discoloration, well-supported fat and smooth transitions between aesthetic subunits.
In contrast, superficial signs of aging in the inferior periorbita include changes secondary to ciliary lesions such as varying degrees of rhytitis, keratoses development, and dyschromias. In general, there is no excessive abundance of lower eyelid skin, and excessive resection can lead to poor lid positioning.
The supporting structures of the lower eyelid also succumb to age and gravity, as the tarsus and canthal ligaments become less elastic causing increased scleral appearance and lid displacement. The orbicularis oculi and septum orbitale also become more lax and redundant, allowing the formation of festoons and pseudoherniation of the orbital fat. To demonstrate this looseness, the lid rebound test should be performed to determine the need for lid support. A positive test is confirmed when a second or more has elapsed before the eyelid returns to its resting position in the eye after maximal forward distraction.
Clinically meaningful quantitative measures of lower lid laxity include intraoperative eyelid distraction greater than 3 mm above the lateral orbital rim or 6 mm anterior distraction away from the globe.
[33] If lower lid laxity is confirmed on examination, an adjunctive procedure should be incorporated into the operative plan to provide lower lid support.
The surrounding periorbital architecture is equally important in determining the indication for lower lid support. Notably, the relationship between the anterior projection of the globe, the lower eyelid, and the malar, as described by Jelks and Jelks, is a key element in the preoperative assessment (see image below).
[34] The patient with a negative carrier relationship is predictably, morphogenically prone to postoperative malposition of the lower eyelid. This relationship exists when the most anterior prominence on the planet is in front of the lower orbital rim. Thus, a negative vector relationship is an indication to include surgical maneuvers for lower eyelid support.
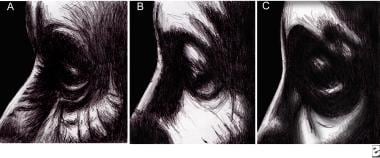
A. Positive vector B. Neutral vector C. Negative vector relationships between the sphere and the orbit.
The patient with a protruding globe is also morphogenically prone to lower lid malposition postoperatively unless recognized preoperatively and treated intraoperatively.
[35] Similar to evaluating the negative vector relationship, sphere protrusion is determined by evaluating the position of the sphere relative to the trajectory. Multiple systems are available, however the Hertel exophthalmometer is most commonly used. It measures the distance between the most anterior prominence of the globe and the lateral orbital rim. Although there are ethnic differences, a sphere projection between 15 and 17 mm is considered within normal limits.
[36] In cases where the projection of the globe is greater than 18 mm, special considerations and surgical maneuvers are required when dealing with the lateral canthus to avoid malposition of the lower lid, sclera, and ultimately dry eye syndrome. Hirmand et al., provide an excellent description of the management of these challenging cases.
[37]
Among other important factors to evaluate is the relative lack or excess of retrodiaphragmatic fat. With the patient in an upright position, the amount of retrodiaphragmatic fat can be observed, combined with gentle measurement of the globe to determine which compartments contain excess fat. While a lack of fat will exclude fat resection from the surgical plan, excess fat can be removed or repositioned to smooth the transition of the eyelid junction to the cheek.
A limited ophthalmologic examination should also be performed, including visual acuity, evaluation for visual field deficits, and extraocular motor function. If significant deficits are present, the patient should be referred for ophthalmologic evaluation.
Finally, a photographic file documenting the preoperative periorbital anatomy should be created. We recommend obtaining a frontal and lateral view of the full face along with close-up views of the periorbital region with the eyes in neutral and upward gaze. Not only are these photographs an important part of the medical record, they can facilitate discussion of the patient’s anatomical problems and what can realistically be treated.