September 18, 2024
4 minutes reading
Basic foods:
- Oral bacteria can spread to the lungs, affecting respiratory health.
- Periodontal treatment included cleaning and 2 weeks of chlorhexidine treatment.
- There were no improvements in spirometry measurements.
The next time you have patients struggling with airway resistance, you may want to refer them to your local periodontist for a deep cleaning, according to a poster presented at the European Respiratory Society International Conference.
“The concept of the ‘mouth-lung axis’ has gained more attention in recent decades, linking oral health to respiratory health.” Anders Røsland, a PhD candidate in the department of clinical dentistry at the University of Bergen in Norway, told Healio.
The mouth-lung axis
Oral bacteria can migrate from the mouth to the lungs, potentially causing or worsening respiratory conditions, Røsland said.


Anders Røsland
“In diseases like periodontitis, we know that the abundance of pathogens is significantly higher compared to healthy individuals,” he said.
Current evidence linking periodontitis to respiratory disorders is largely epidemiological, although some interventional studies focus primarily on patients with COPD, he continued.
“These intervention studies have shown beneficial results, including improved lung function and reduced exacerbation rates after periodontal interventions,” said Røsland.
In the current trial, researchers investigated the effect of improved oral health through periodontal treatment in otherwise healthy individuals.
“This would help us understand the potentially causal and preventive role of proper oral care in respiratory health, as no previous study has investigated this relationship in non-smokers without pre-existing respiratory conditions,” said Røsland.
Time to clean up
The study included 62 patients (mean age, 35.8 years, 63% female) with periodontitis (stage 1, 21%; stage 2, 79%) who were nonsmokers and otherwise healthy.
“Periodontitis is a chronic inflammatory disease of infectious origin that affects the tissues surrounding the teeth,” said Røsland.
Periodontitis is characterized by the progressive loss of connective tissue and bone caused mainly by chronic inflammation caused by the persistent presence of pathogenic bacteria in dental biofilms.
“These bacteria accumulate in the periodontal pockets, leading to the activation of the body’s immune response, which leads to the breakdown of the supporting structures of the teeth—and ultimately, tooth loss,” Røsland said.
The researchers conducted a periodontal examination on each patient, which included a detailed medical history to assess whether any comorbidities might affect the patient’s periodontal health.
“The clinical examination includes the assessment of the depth of the periodontal pockets, the level of inflammation in the gums (bleeding on probing) and the level of oral hygiene as measured by the plaque score,” said Røsland. “In addition, an X-ray is taken to assess the extent of bone loss.”
Periodontal treatment, which each patient also received, included education about oral hygiene practices and a whole-mouth disinfection protocol to reduce gingival inflammation and oral bacterial load to control the progression of periodontitis. The stepwise approach followed the guidelines of the European Federation of Periodontology.
“The process starts with informing the patient about their diagnosis and creating an individualized treatment plan,” said Røsland.
She is educated on proper oral hygiene techniques, including brushing, flossing, and using interdental brushes to maintain plaque control at home.
“This helps manage plaque build-up, which is a major contributor to periodontal disease,” said Røsland. “Patients are provided with a complete kit of oral hygiene agents to help them maintain oral hygiene.”
Immediately, patients then received a deep cleaning, which involved mechanically removing biofilm from the teeth both above and below the gum line.
“This includes the elimination of plaque, calculus and bacterial toxins from tooth surfaces and periodontal pockets,” said Røsland. “Additionally, root planing smoothes root surfaces to prevent bacterial build-up, promoting gingival reattachment to teeth and reducing pocket depth.”
Patients then followed a 2-week regimen of 0.2% chlorhexidine oral solution and 1% chlorhexidine gel.
Study results
The researchers measured lung function via spirometry and pulsometry at baseline and at 3 and 6 weeks. Periodontal health was assessed again at 6 weeks and the investigators reported improvements in all periodontal parameters.
There were no improvements in spirometric measurements, including FEV1forced vital capacity (FVC) or FEV1/FVC ratio.
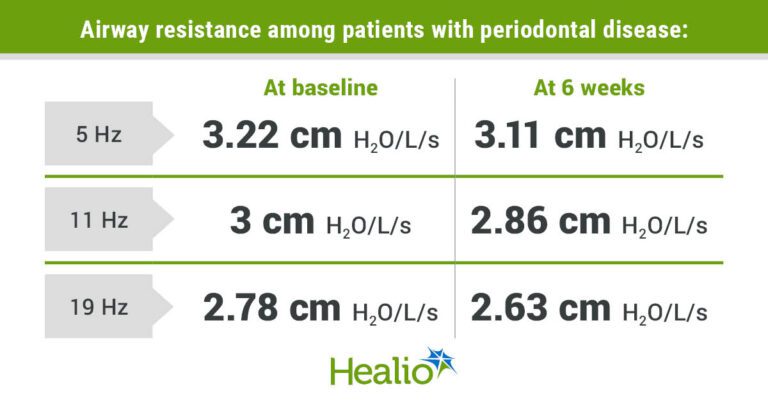
However, airway resistance decreased by 4.7% from 3 cm H2O/L/s up to 2.86H2O/L/s (P = .003) at 11 Hz and by 5.4% from 2.78 Hz2O/L/s up to 2.63H2O/L/s (P = .002) at 19 Hz. Airway resistance was also reduced by 3.4% from 3.22H2O/L/s to 3.11H2O/L/s at 5 Hz, but the researchers did not find it statistically significant.
“Almost half of the patients showed improved airway resistance,” said Røsland. “A reduction in airway resistance suggests that patients experienced less obstruction in their small airways, leading to easier breathing.”
Noting that these improvements were seen within just 6 weeks, Røsland said it will be important to assess the durability of the airways over a longer period of time.
Next steps
Lung diseases such as asthma and COPD can be treated but not cured, Røsland said, which makes prevention crucial.
“By making a connection between periodontal disease and lung health, we believe there is a strong rationale for implementing an oral hygiene program that improves both oral and respiratory health,” said Røsland.
Existing evidence suggests that doctors should refer patients with lung disorders or those at risk for oral and periodontal health screenings, he continued.
“We believe that this approach, with collaborative efforts between health care providers, could contribute to the prevention of respiratory diseases and other conditions associated with poor oral health,” said Røsland.
Next, he continued, researchers should conduct large-scale, long-term randomized clinical trials to strengthen the existing evidence.
“Furthermore, detailed characterization of the oral microbiome, focusing on specific bacterial compositions and functional genes that could potentially predict respiratory outcomes, would be important for developing patient-tailored treatment plans,” he said.
“In addition, assessment of systemic inflammatory markers in these patients would be of interest, as both periodontitis and respiratory disorders are associated with systemic inflammation,” he said.
For more information:
Anders Røsland you can contact anders.rosland@uib.no.