INTRODUCTION
Replacing an entire arch of failing teeth has long been considered the panacea of implant dentistry. The All-on-4 protocol as described by Malo et al1 has shown excellent implant and prosthetic success rates. Traditional analog workflows included:
- Preliminary diagnostic impressions
- Diagnostic test setup
- Surgical procedures, including analog impressions
- Test/bite confirmations
- Placement of temporary prostheses
These additional steps increase the overall time required to deliver the intent as well as the cost. Continued development in additive manufacturing (3D printing) has led to predictably accurate prints. Resins used in modern 3D printing have been shown to have physical properties similar to milled polymethyl methacrylate (PMMA)2 and can now be printed on “desktop” printers.
In addition to the improved speed and accuracy of 3D printed restorations, the application of photogrammetry allows the precise mapping of implant positions, ensuring the delivery of a completely passive prosthesis.3
The use of CAD software (exocad) allows the rapid production of a digital file, which, when combined with all relevant preoperative and intraoperative data, allows the clinician to quickly approve the case design and proceed with the fabrication of the prosthesis. This case report describes a simplified, all-digital workflow to provide a full-arch temporary prosthesis within 24 hours.
CASE REPORT
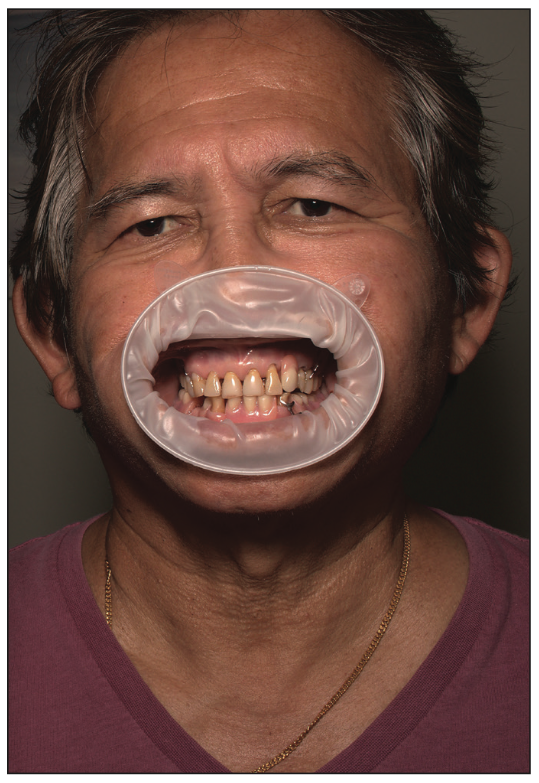
A patient presented with a partially edentulous mandible and a failed acrylic lower partial denture (Figure 1) and requested a fixed solution with the specific desire to “be able to bite into an apple”. The existing vertical dimension of occlusion (VDO) was satisfactory and the initial CBCT was performed with the patient in occlusion at this VDO (Figure 2). This preoperative CBCT will provide a reference to correlate the postoperative CBCT with the patient’s initial vertical dimension. If any lesions are anticipated, it is important that they be performed prior to diagnostic CBCT either by adding composite material to existing teeth in edentulous patients or by fabricating a denture in the correct VDO in edentulous patients.
Figure 1. The patient presented with a partially dentate mandible and malformed teeth Nos. 22 and 27.
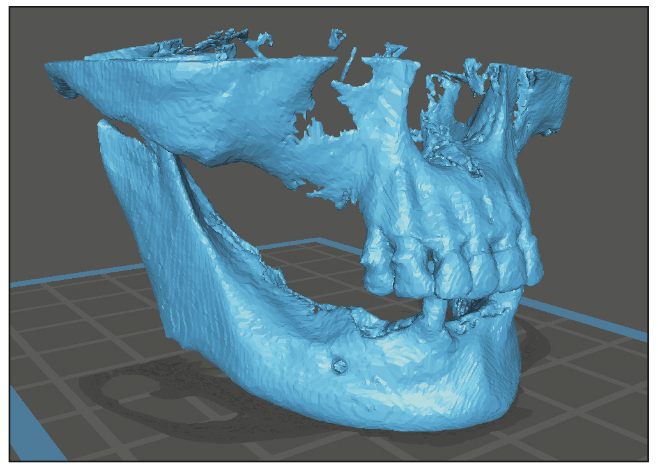
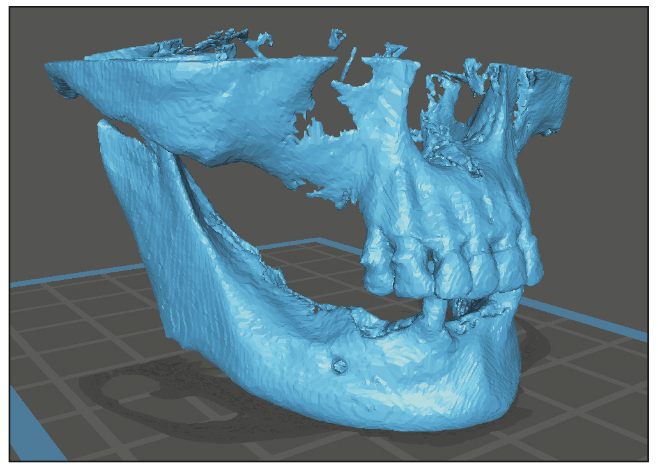
Figure 2. Preoperative CBCT obtained to document initial vertical dimension.
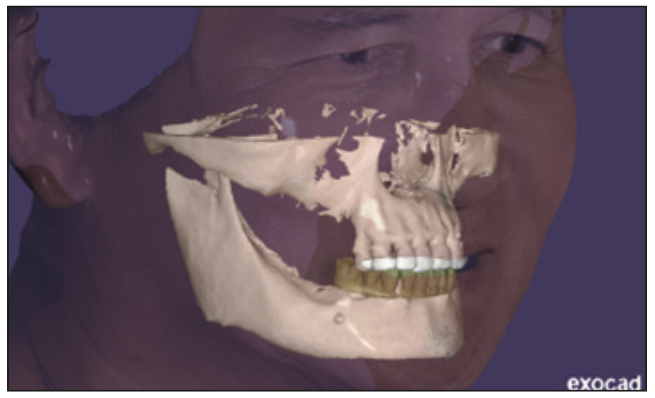
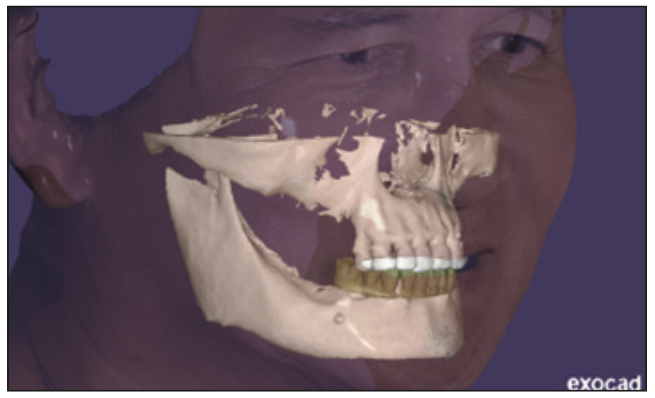
Figure 3. The exocad drawing file.
Additional diagnostic data collected at this appointment included intraoral scans (i700 [Medit]), DSLR photography and 3D face scanning (Vectra Smile [JK Dental Group]). All diagnostic data were merged in exocad to create a digital patient (Figure 3).
Implant planning was performed using the Blue Sky Plan (BlueSkyBio) planning software to ensure that there was sufficient bone available for placement and immediate loading of the implants (Figure 4). Freehand surgery was performed on the patient under IV sedation.
After completion of surgery and prior to surgical closure, iCam body scans were performed using Imetric 4D Imaging photogrammetry (Figures 5 through 7).
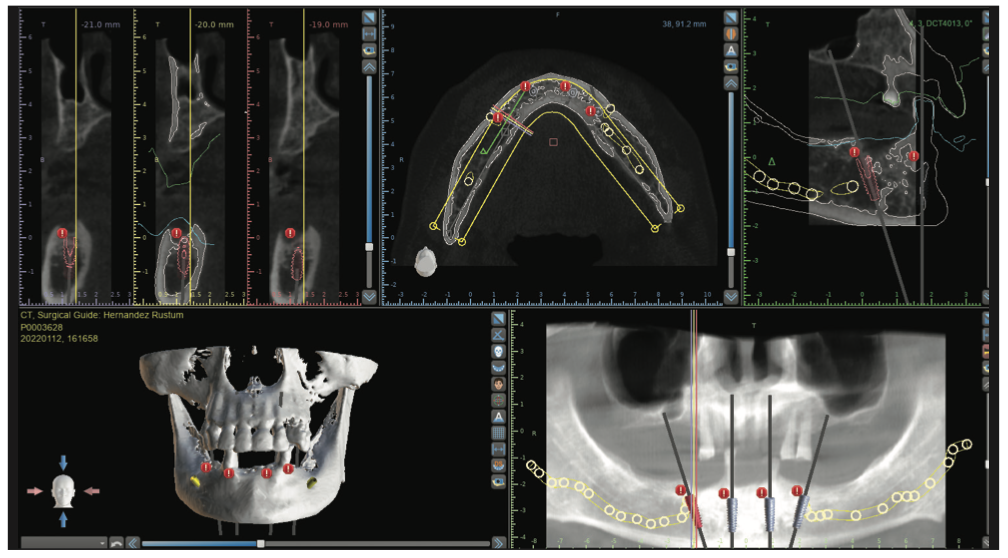
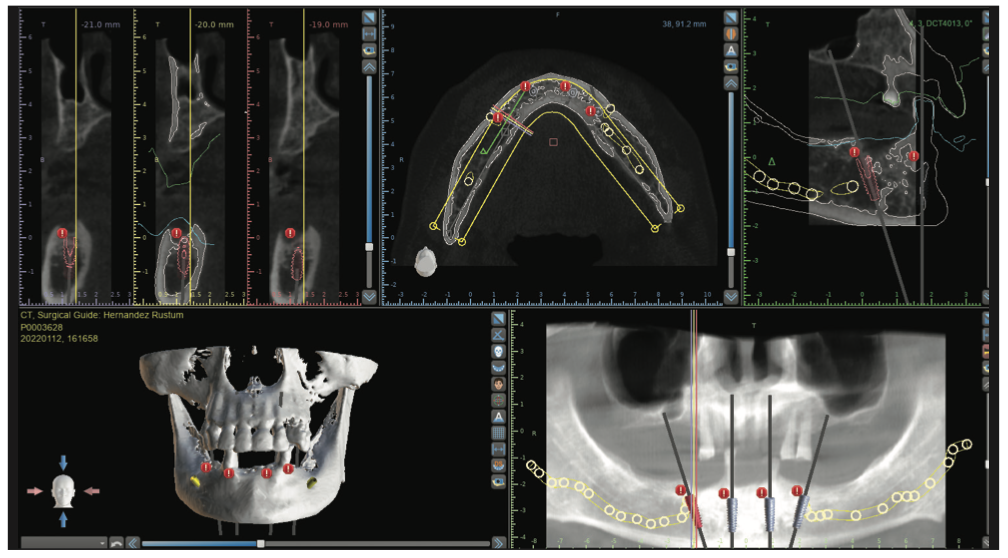
Figure 4. Surgical planning in Blue Sky Plan (BlueSkyBio) planning software.
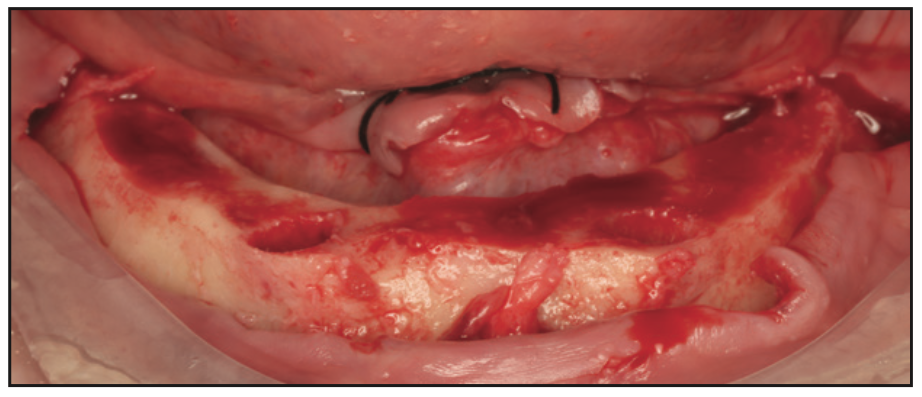
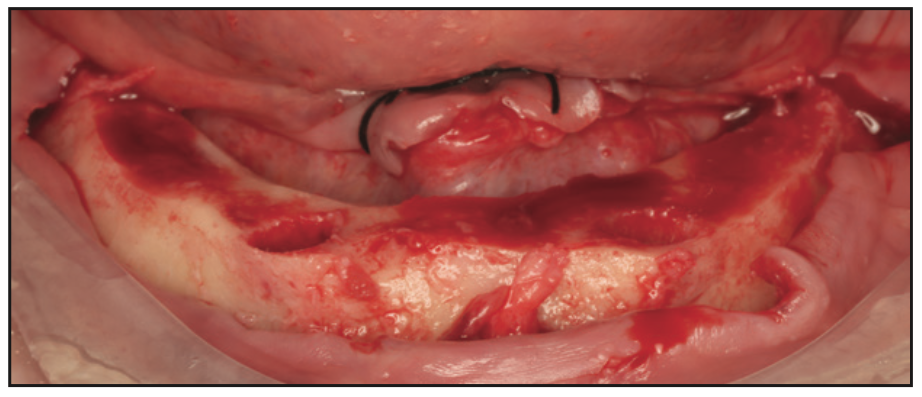
Figure 5. Jaw after alveectomy for prosthetic space.
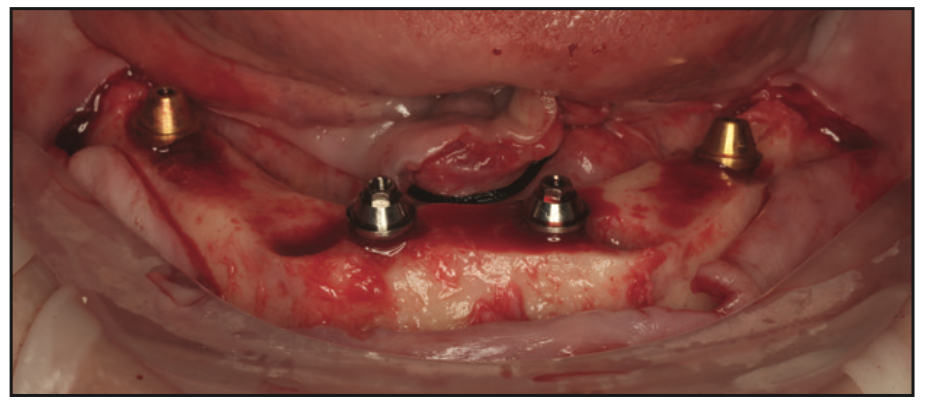
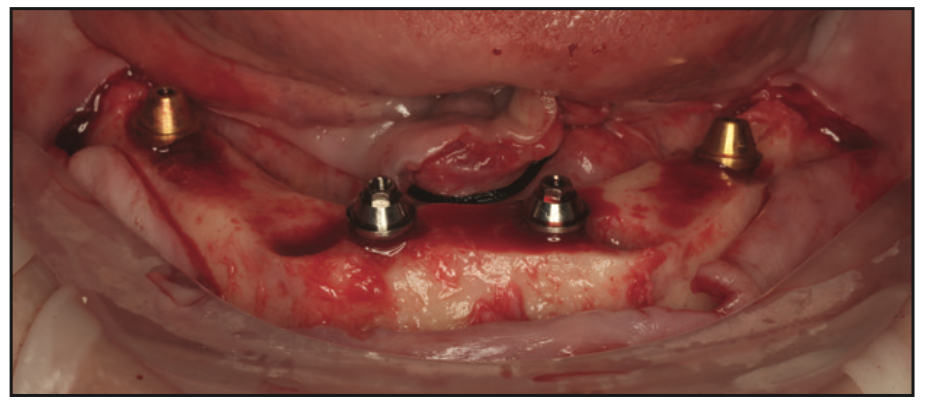
Figure 6. Implants placed.
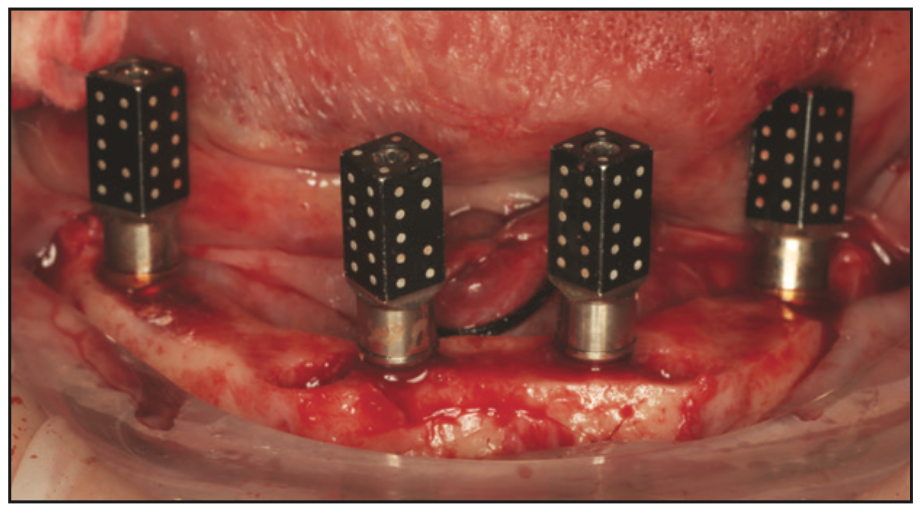
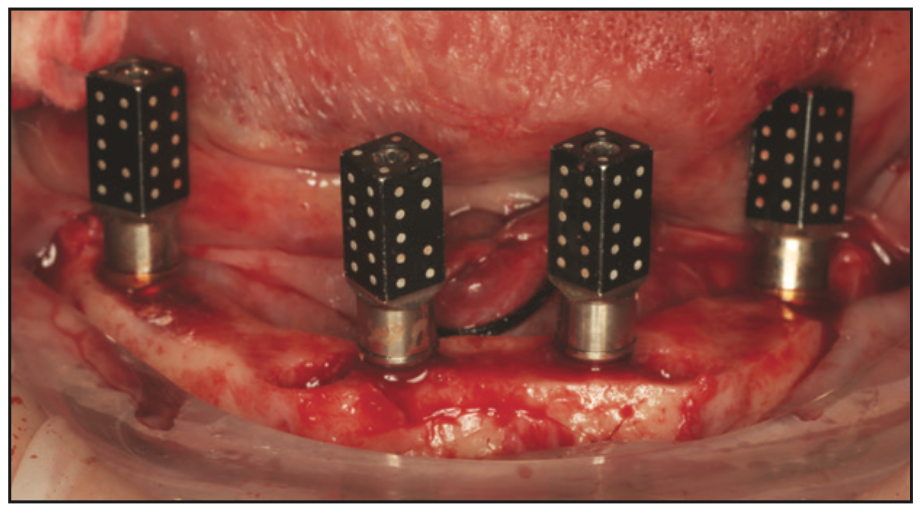
Figure 7. Implants with attached iCam (Imetric 4D Imaging photogrammetry) body scans.
A post-operative CBCT scan was performed to create 2 STL files from DICOM data by changing the thresholds:
- An STL of iCam reference bodies for suturing in soft tissues (increasing the Hounsfeld unit limit).
- A hard tissue STL for correlation with CBCT prior to operation within the Imetric software (reducing the Hounsfeld unit limit).
All diagnostic data were aligned and exported to exocad to create an STL file of the temporary prosthesis.
The prosthesis was designed in exocad CAD software (Figures 8 and 9) and 3D printed on an Ackuretta Sol printer using Rodin Sculpture A1 Resin (Pac-Dent) following the manufacturer’s settings. The optimal support settings were created by the AI software.
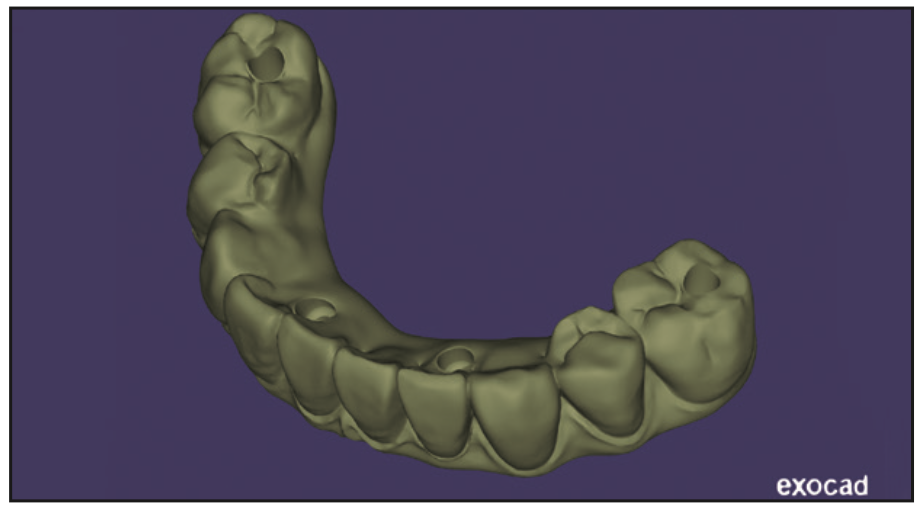
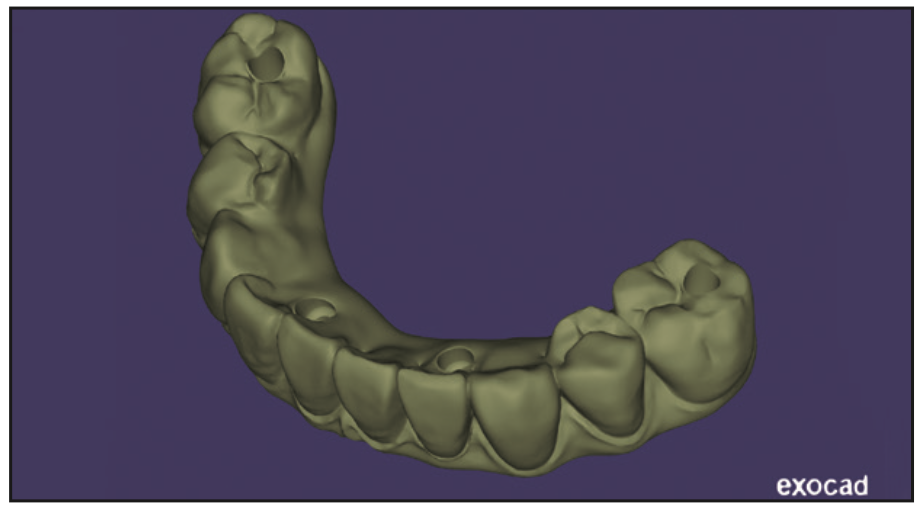
Figure 8. Prosthesis design.
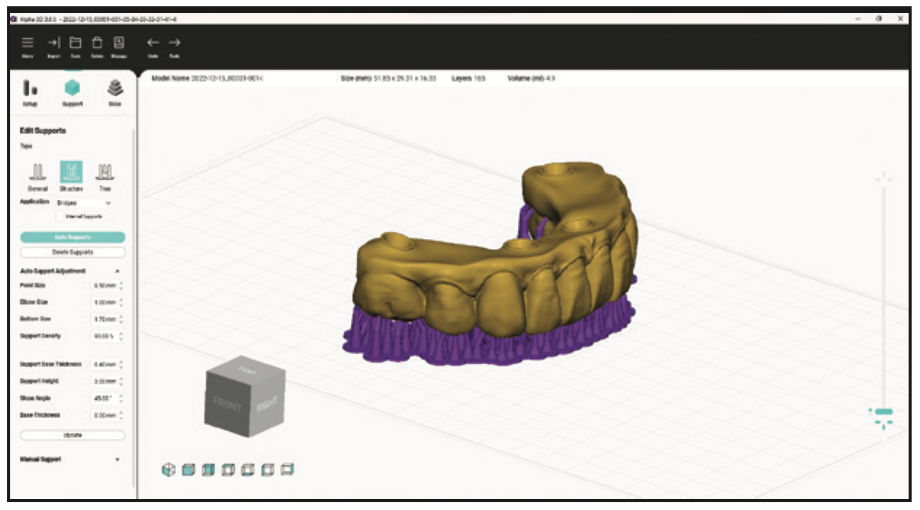
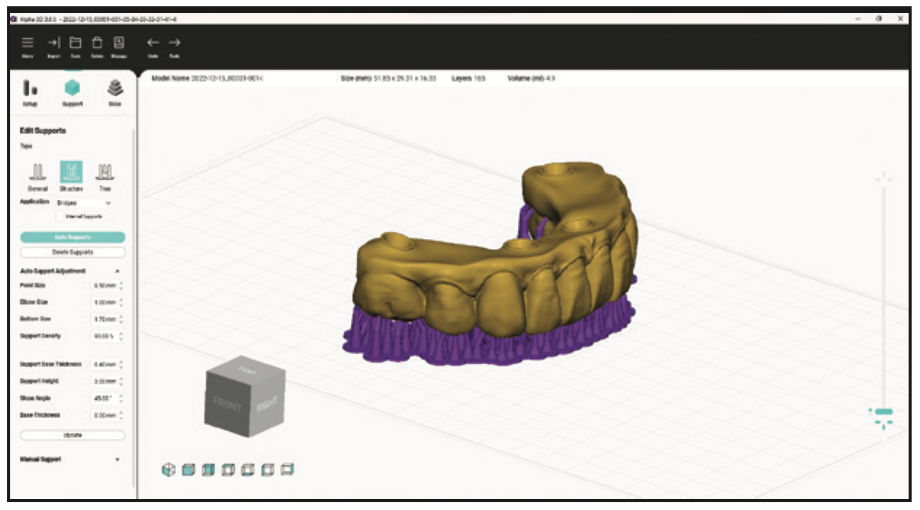
Figure 9. Embedding in print software.
Rodin Sculpture (Figure 10) is a new ceramic nanohybrid resin that streamlines the fabrication process while reducing fabrication costs for both clinicians and dental laboratories. It is an FDA 510(k) cleared, biocompatible, light-curing resin designed for use with specific CAD/CAM systems in conjunction with manufacturer-validated 3D printing and light-curing devices. This new resin can be used to make permanent full contour crowns, inlays, inlays and veneers. In addition, it can be used to fabricate direct All-on-X prostheses, monolithic dentures, and split-file dentures. It consists of the same resin components found in most restorative composites with the addition of a high concentration of true nanoceramic fillers that provide brilliant radiolucency.
Rodin was chosen for its excellent mechanical properties combined with its vivid translucency. It offers the highest strength and flexural modulus of any long-term/permanent restoration and has realistic aesthetics. It is also extremely resistant to breakage, reducing the frequency of repairs and rebuilds.
After printing, the prosthesis was removed from the build plate and the supports were removed (Figures 11 and 12). It was then carefully washed with isopropyl alcohol to remove excess uncured resin. The mounting edges were finished smoothly with a low-speed handle and finish. The denture was then polished with pumice stone and acrylic polish for a final finish.


Figure 10. Rodin sculpture (Pac-Dent).
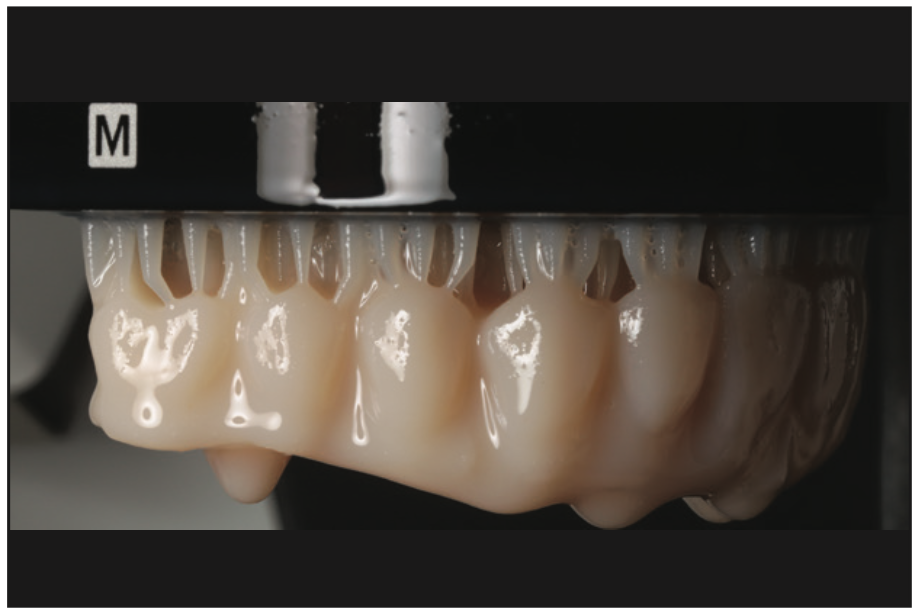
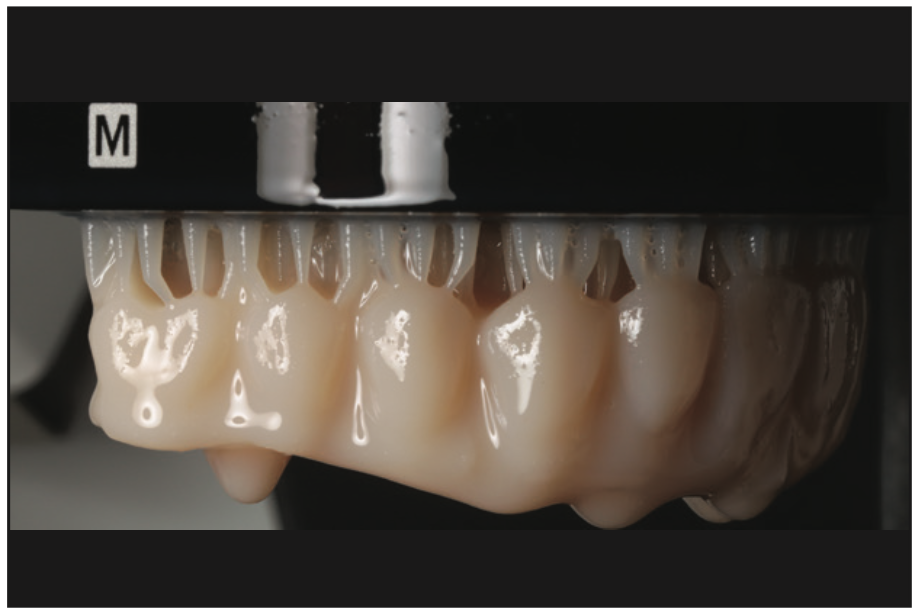
Figure 11. Printed prosthesis on build plate.


Figure 12. Prosthesis before cleaning.
Gum staining and vitrification was achieved using Larry’s Magical Denture Elixirs [TAUB Products]) and Rodin Palette glaze for characterizing surfaces (Figure 13). The graft was then photocured in the Accuretta Curie unit.
The following morning, the temporary prosthesis was delivered with polymer-specific prosthetic screws. No closed fitting was required. During the design of the prosthesis, care was taken to minimize the length of the cantilever and to maintain the minimum thickness around the implant access channels.


Figure 13. Staining and vitrification of the prosthesis.
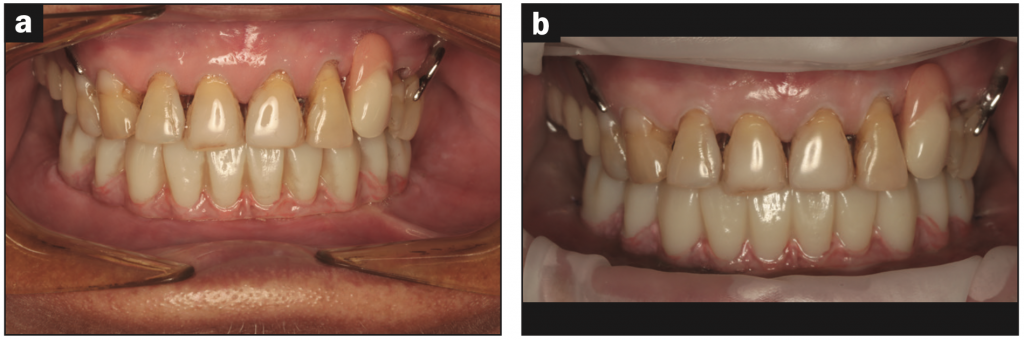
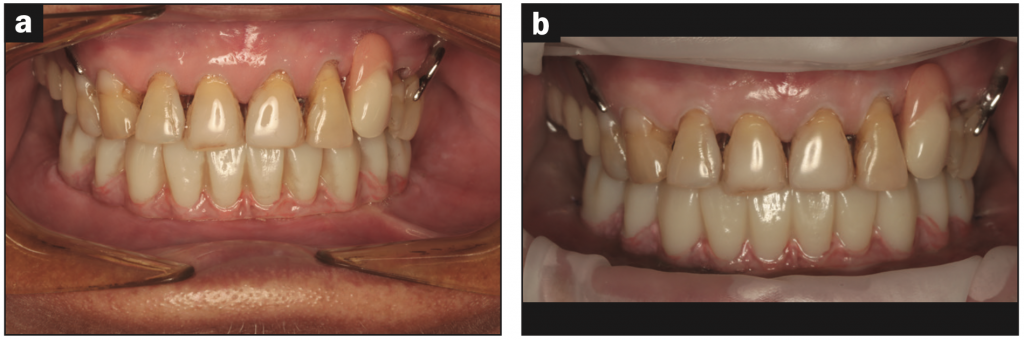
Figure 14. (a) Provisional prosthesis at initial delivery and (b) at 6 months in service before proceeding with definitive restoration.


Figure 15. Intraoral condition before the definitive restoration.
The photographs in Figure 14 show the temporary prosthesis at delivery and in operation for 6 months before proceeding with the definitive restoration. Figure 15 shows the healing under the printed bridge, which demonstrates the biocompatibility of the Rodin material.
BIBLIOGRAPHICAL REFERENCES
1. Malo P, de Araújo Nobre M, Lopes A, et al. A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc. 2011? 142 (3): 310–20. doi:10.14219/jada.archive.2011.0170
2. Alageel O, Alsadon O, Almansour H, et al. Assessment of the effect of accelerated aging on temporarily fixed dental materials using digital technologies. J Adv Prosthodont. 2022? 14 (6): 360–8. doi:10.4047/jap.2022.14.6.360
3. Ma B, Yue X, Sun Y, et al. Accuracy of photogrammetry, intraoral scanning, and conventional impression techniques for complete restoration of arch implants: an in vitro comparative study. BMC Oral Health. 2021? 21(1):636. doi:10.1186/s12903-021-02005-0
ABOUT THE AUTHOR
Dr. O’Dowling graduated from University College Cork, Ireland, in 2006, where he was awarded the Noel Hayes Award for Oral Surgery and the British Undergraduate Society Award for Restorative Dentistry, and was accepted as a Fellow of the American Dental Association’s Student Clinicians for project work on hypomineralization of molars/sectors. He has worked in private practice in Ireland and in Queensland and Perth, Australia. During this time, he continued to further his knowledge in implant surgery and prosthetics and completed his MSc in Oral Implantology in 2018 from Goethe Dental School (Frankfurt, Germany). He is a Diplomate of both the International Congress of Oral Implantologists and the American Board of Oral Implantology/Implant Dentistry and a Fellow of the American Academy of Implantology. Dr. O’Dowling maintains a keen interest in all aspects of implantology, ranging from simple implant placement to advanced techniques such as partial extraction therapy, autogenous bone plates and sinus augmentations. His current focus is on simplifying full arch restoration protocols using digital techniques and 3D printing. He can be reached at daveodowling83@gmail.com.
Disclosure: Dr. O’Dowling reports no disclosures.