INTRODUCTION
After traumatic injuries to the teeth, such as dislocation or avulsion, stabilization is paramount. Requirements for braces include:
- Passive, not active, force on a tooth
- Allows normal tooth movement
- No soft tissue damage
- It does not adversely affect the occlusion
- Allowing endodontic treatment to be carried out if needed
- A tooth that is easy to clean
- Ease of removal from the tooth1.2
The most common treatment is the use of a flexible splint. Different materials are used and the treatment is basically the same.3 Another treatment to stabilize the tooth after extraction is to staple the tooth in place.4 Bleeding is often present and blood, as well as saliva, will make adhesion between the teeth and any resin difficult. Pediatric patients are often tearful and fearful, and it can be difficult to deal with the lingering trauma of a long dental appointment. One should treat the traumatic tooth as quickly and succinctly as possible.
Methods
This is the current protocol we use in these cases:
- Stabilize the tooth with light-cured resin (Light Fix [Sun Medical Co Ltd])
- Make an impression
- Create a vacuum formed retainer (hard type, 1.0 mm thick)
- Deliver the retainer within 8 hours of the injury
- Keep retainer all day except brushing teeth (28 days)
- Check tooth mobility after 1, 7, 14 and 21 days
- In case of dislocation, take electric pulp test (EPT) (scale 1 to 10) after 1, 7, 14 and 21 days
- Check tooth mobility, impact, palpate and probe and take EPT and periapical X-ray after 28 days
CASE REPORTS
Case 1
The patient was a 5-year-old girl who fell over a water bottle while drinking and dislodged her deciduous left lateral incisor. The child care worker washed her tooth with tap water and cleaned the dirt from the tooth, removing the periodontal membrane. The tooth was replanted and stabilized with light-cured resin and an impression was taken. He returned to the dental clinic 3 hours later and received a vacuum-formed retainer. Her mother was instructed that her daughter should wear the retainer all day except when brushing her teeth. The tooth was checked after 1, 7, 14 and 21 days and a tooth x-ray was taken after 28 days. The endodontic treatment was done after the tooth was stable. The 12-month follow-up was within normal limits (Figure 1).
Figure 1a. Preoperative intraoral photograph.
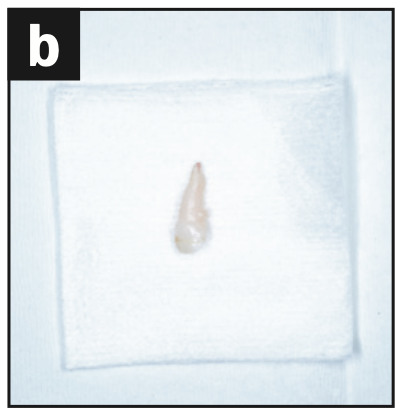
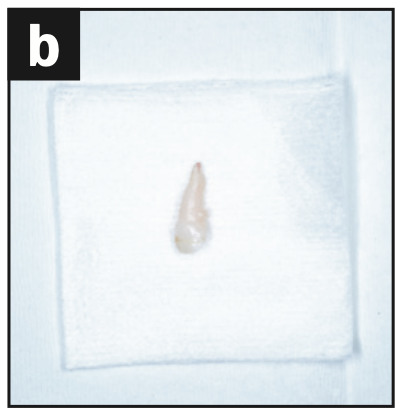
Figure 1b. Dislodged tooth


Figure 1c. Intraoral photo? the tooth was replanted and fixed with light-cured resin.
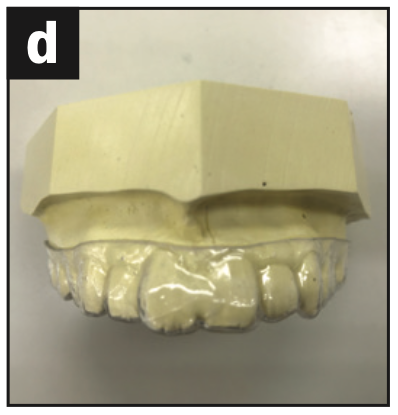
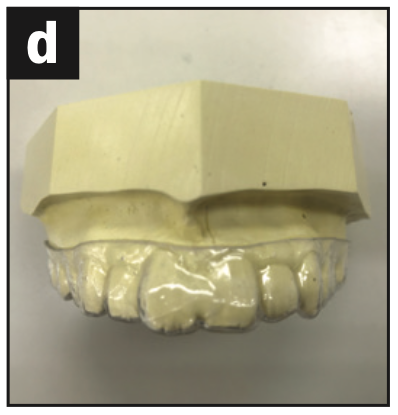
Figure 1d. Vacuum-retained working model.


Figure 1e. Intraoral photograph wearing the vacuum-formed retainer.


Figure 1f. Intraoral photograph at 28 days postoperatively.


Figure 1g. Preoperative X-ray.


Figure 1. Radiograph immediately after replantation.


Figure 1i. X-ray 28 days after surgery.


Figure 1j. Root canal filling radiograph.


Figure 1 Mr. Intraoral photograph 12 months after surgery.


Figure 1l. X-ray at 12 months after surgery.


Figure 1m. Intraoral photograph 18 months after surgery.


Figure 1n. X-ray at 18 months after surgery.
Case 2
This patient was a 24-year-old woman. It had fallen causing a lateral dislocation of the left maxillary central incisor. The next morning, it came to the office, where it was fixed with a light-cured resin, and an impression was left. Six hours later, he returned and received a vacuum-formed retainer. She was instructed to wear the retainer all day except for brushing her teeth. Susceptibility tests were performed after 1, 7, 14 and 21 days. Tooth mobility and palpation were checked, EPT was performed and tooth x-ray was taken after 28 days. The tooth had +1 mobility in the labial-palatal direction and no reaction to EPT. Three months later, the tooth was restored and responded to EPT (8/10). At the 4-month recall, the tooth responded to EPT (4/10). At 5 months, a sinus tract was noted. The tooth did not respond to EPT. An x-ray showed damage to the apex. The diagnosis was pulp necrosis and root canal treatment was done in 2 visits. One month later (6 months after the appearance of the wound), the venous tract disappeared and the radiograph showed the healing process (Figure 2).


Figure 2a. Preoperative intraoral displacement photograph.


Figure 2b. Preoperative displacement radiograph.


Figure 2c. Intraoral photograph of the replanted tooth.


Figure 2d. Intraoral photograph. The tooth was fixed with light-cured resin.


Figure 2e. Working model with molded vacuum retainer.


Figure 2f. Intraoral photograph. Wearing a vacuum formed retainer.
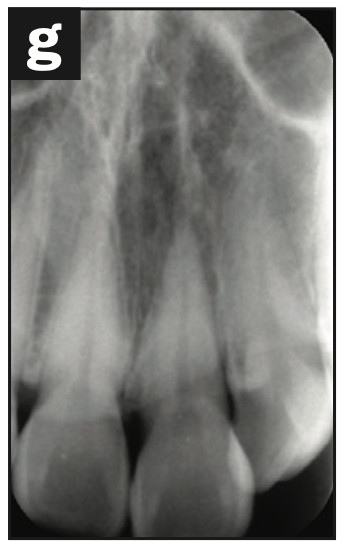
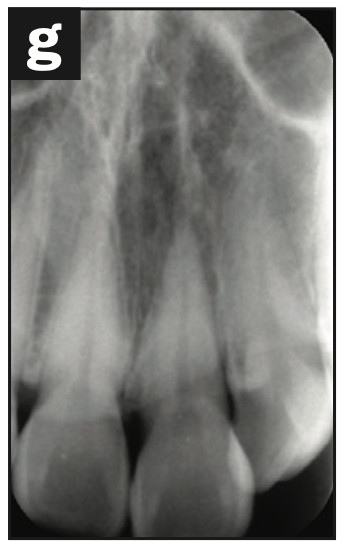
Figure 2g. Radiograph immediately after replantation.


Figure 2h. Intraoral photograph 28 days after surgery.
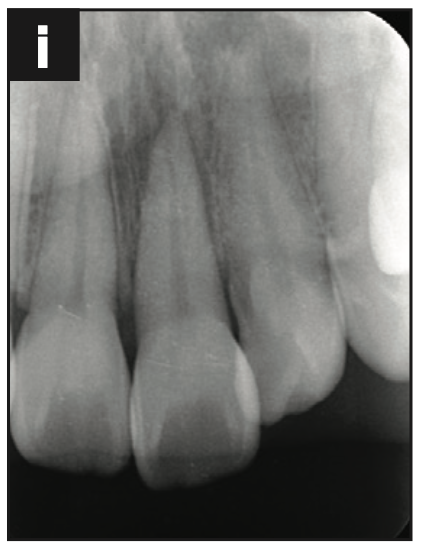
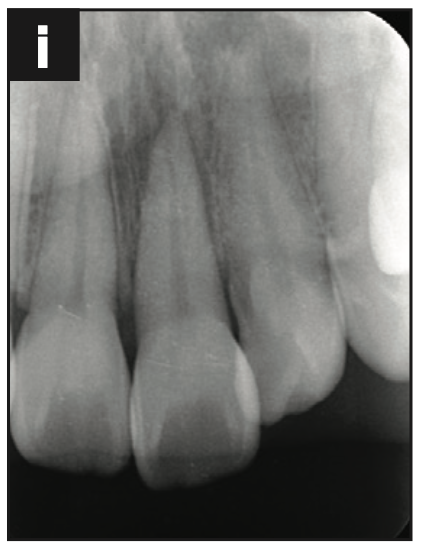
Figure 2i. X-ray 28 days after surgery.


Figure 2j. Intraoral photograph 3 months after surgery.
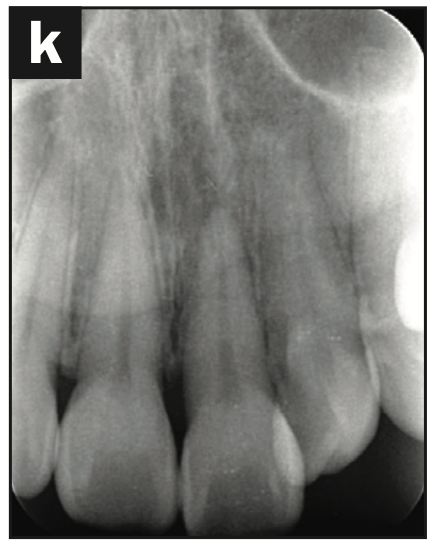
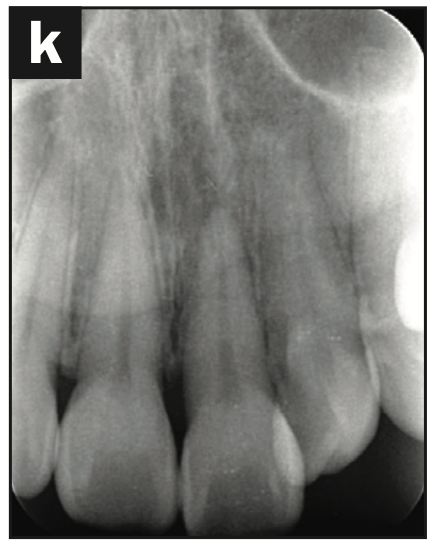
Figure 2 Mr. X-ray 3 months after surgery.


Figure 2l. Intraoral photograph 5 months after surgery. venous access was present.
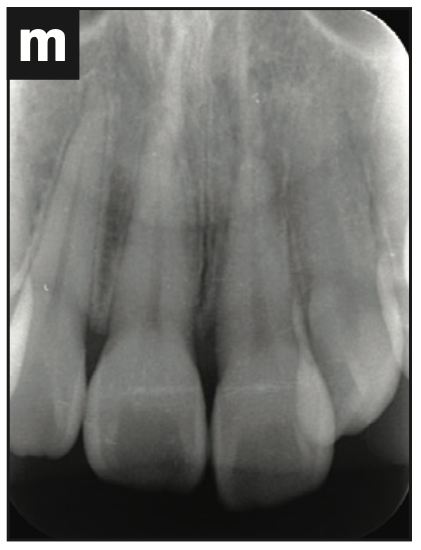
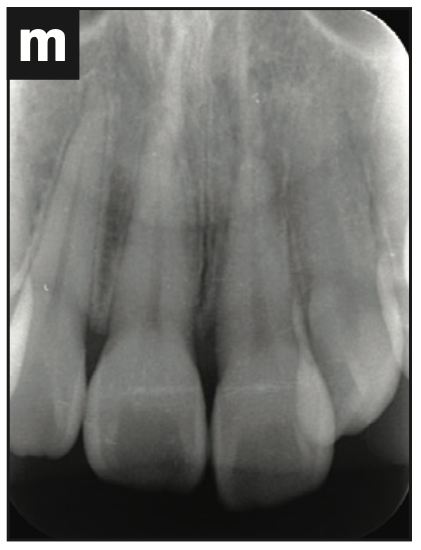
Figure 2m. X-ray at 5 months after surgery. the tip of the tooth had a lesion.


Figure 2n. Intraoral photograph 6 months after surgery. the venous line was gone.
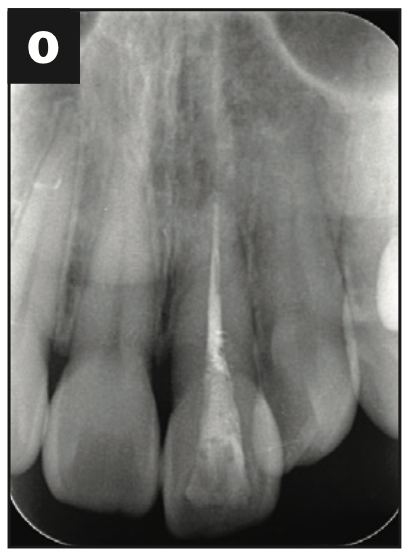
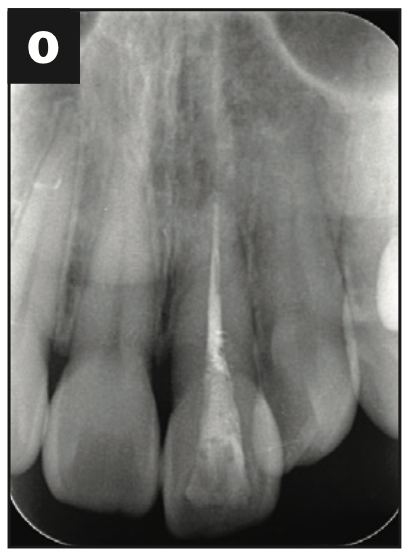
Figure 2o. X-ray at 6 months after surgery. the apex of the tooth shows healing.
Case 3
A 42-year-old woman fell causing palatal dislocation of the maxillary left central incisor. An alveolar bone fracture on the palatal side was seen on CBCT. The fracture was reduced and fixed with light-cured resin and an impression was taken. Two hours later, she returned and was given a vacuum-formed retainer. She was instructed to wear the retainer all day except for brushing her teeth. It was notable that he had a habit of sticking out his tongue. Susceptibility tests were performed after 7 and 28 days. Tooth mobility, EPT, palpation and dental radiographs were obtained after 28 days. At the 28-day follow-up, there was slight tooth mobility and no reaction to EPT. At the 2-month follow-up, the tooth was not discolored, had no mobility, was EPT negative, and was mildly tender to percussion. There was no periapical lesion on radiograph and no sinus tract. At 3-month follow-up, the tooth was responsive to EPT (9/10) and had mild percussion pain. At the 4-month follow-up, the tooth was responsive to EPT (9/10) and no longer sensitive to percussion (Figure 3).


Figure 3a. Preoperative intraoral displacement photograph.


Figure 3b. Preoperative displacement radiograph.
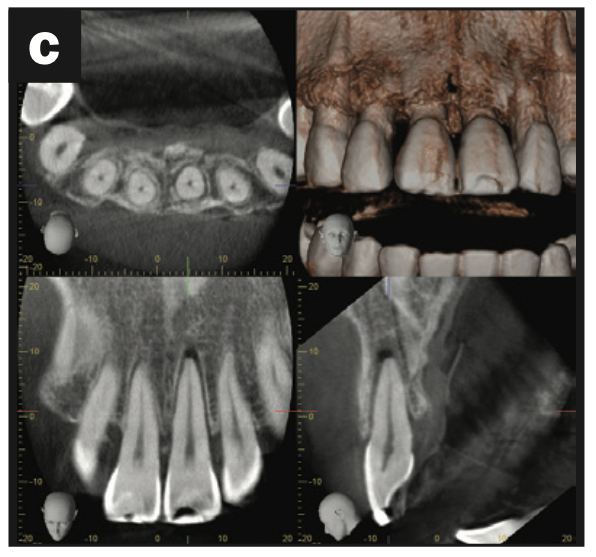
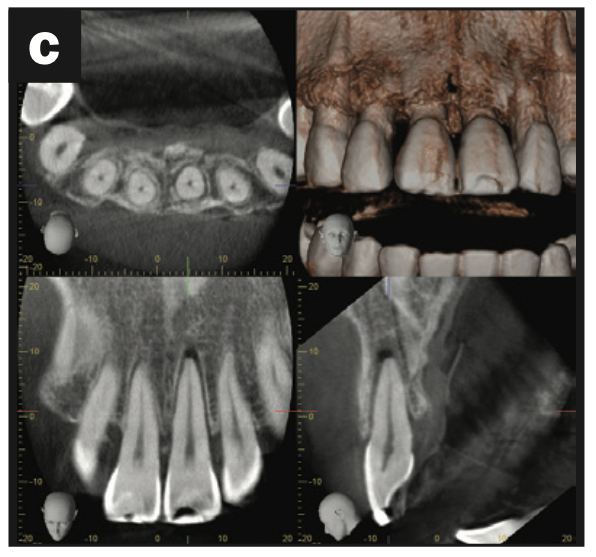
Figure 3c. CBCT scan of the alveolar fracture of the palatal bone.


Figure 3d. Intraoral photograph. The tooth was replanted and fixed with light-cured resin.


Figure 3e. Radiograph immediately after replantation.
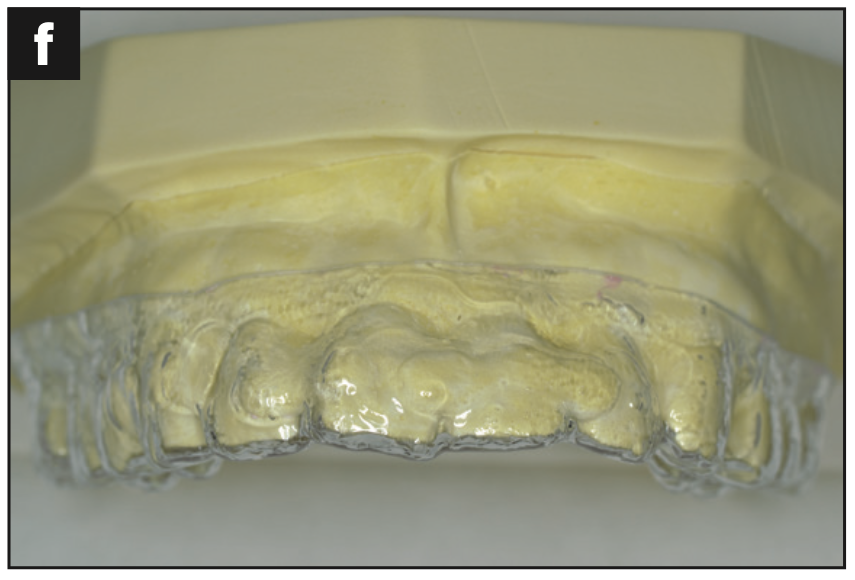
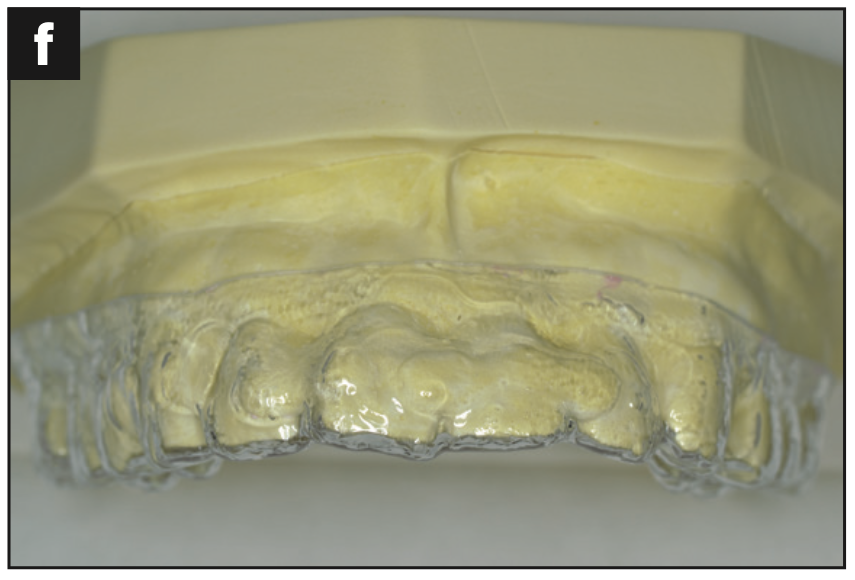
Figure 3f. Working model with molded vacuum retainer.


Figure 3g. Intraoral photograph. Wearing a vacuum formed retainer.


Figure 3h. Intraoral photograph 28 days after surgery.


Figure 3i. X-ray 28 days after surgery.


Figure 3j. Intraoral photograph 3 months after surgery.


Figure 3 X-ray 3 months after surgery.


Figure 3l. Intraoral photograph 4 months after surgery.
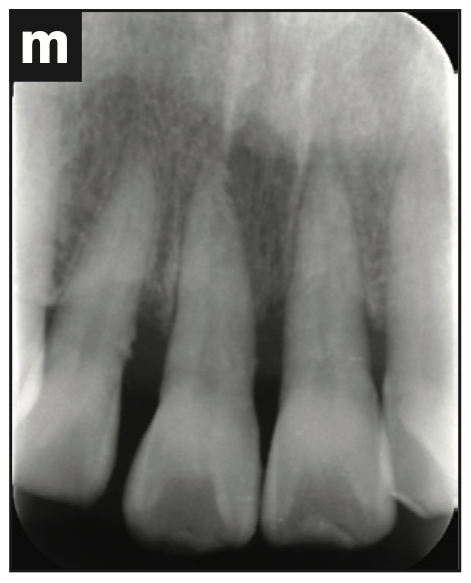
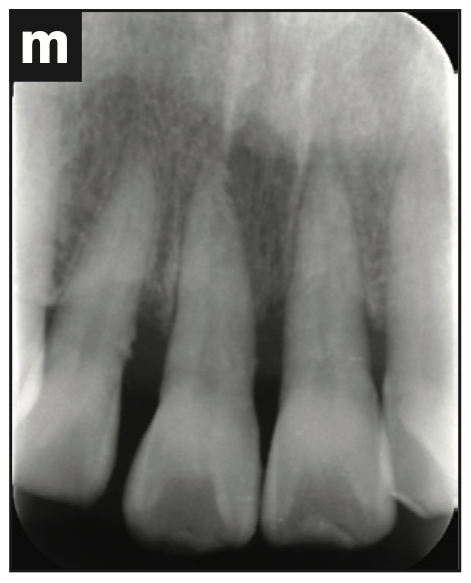
Figure 3m. X-ray 4 months after surgery.
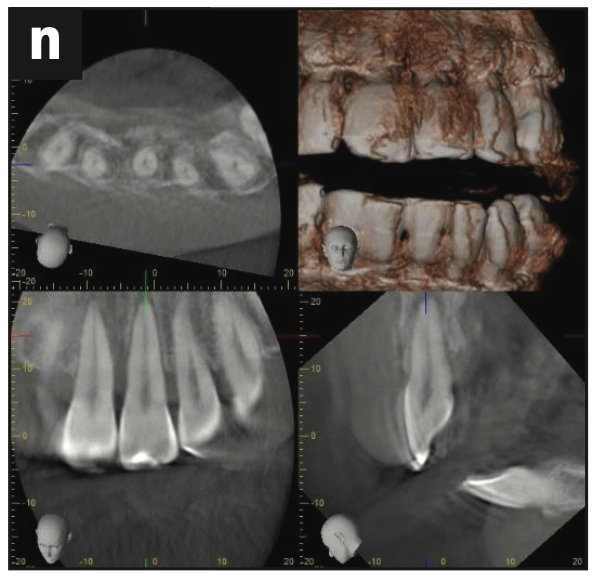
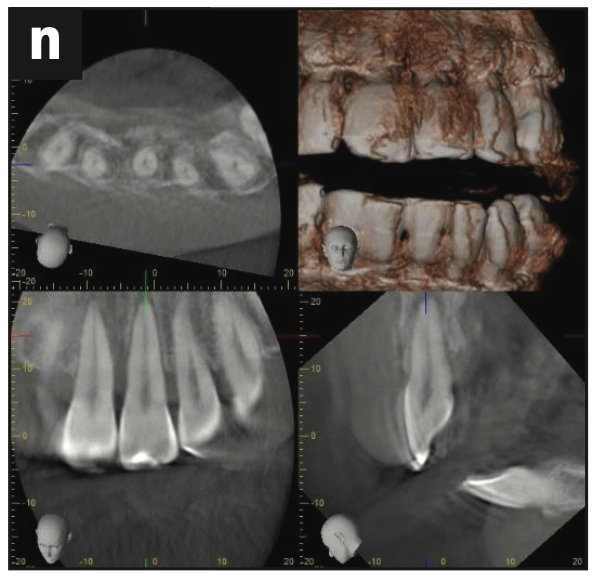
Figure 3n. CBCT scan 4 months after surgery.
DISCUSSION
Trauma patients most often come to the dental office as an emergency. Often they are young patients who are afraid and have difficulty understanding what we are doing as well as following our instructions. Our goals as treating dentists are to remove any infectious substances from the oral cavity and to restore and stabilize swollen, subluxated or detached teeth. It may be difficult at the emergency appointment to reestablish proper resin bonding, but it is critical to obtain an impression in order to create a vacuum pressure retainer. Ideally, a digital impression could be made, which would greatly reduce the chances of further injury to the teeth. The patient and guardian/parent are instructed to wear the vacuum-formed retainer at all times except for tooth brushing for a period of 28 days. The pathological healing process of subluxation, dislocation and dislocation stabilized by the vacuum-formed retainer is the same as using a flexible splint.5,6
The patient in case 1 was young. She ignored the instructions and touched her teeth, removing the resin. The patients of cases 2 and 3 were adults and followed the instructions very well. Adult patients may not require 28 days of immobilization.
CONCLUSION
Traumatic wounds such as dislocation and avulsion stabilized by vacuum-formed retainers (1.0 mm thick) show healing after 28 days if worn continuously except for tooth brushing.
THANKS
Dr. Tsumori would like to thank the staff members of Meiwa Dental Clinic in Japan, Dr. Samuel Kratchman and Dr. Yoshi Terauchi.
BIBLIOGRAPHICAL REFERENCES
1. Andreasen JO, Andreasen FM. Essentials of Traumatic Injuries to the Teeth: A Step-by-Step Guide to Treatment. 2nd edition. Mosby? 2000.
2. American Academy of Pediatric Dentistry Council on Clinical Affairs. Guidelines for the management of acute dental trauma. Pediatr Dent. 2010;32(6 Suppl):202–12.
3. Berman LH, Hargreaves KM. Cohen’s Pulp Paths. 12th edition? Elsevier; 2021.
4. Gupta S, Sharma A, Dang N. Suture splint: an alternative for tooth dislocation injuries in pediatric patients—a case report. J Clin Pediatr Dent. 1997, 22(1):19-21.
5. Sobczak-Zagalska H, Emerich K. Best Splinting Methods in Case of Dental Injury—A Literature Review. J Clin Pediatr Dent. 2020? 44 (2): 71–8. doi:10.17796/1053-4625-44.2.1
6. Baruch H, Ehrlich J, Yaffe A. [Splinting—a review of the literature]. Refuat Hapeh Vehashinayim (1993). 2001? 18 (1): 29-40, 76.
ABOUT THE AUTHORS
Dr. Tsumori He graduated from Tokyo Dental College in 2003 and then served as a clinical assistant at Tokyo Dental College from 2003 to 2004. He is the owner of Meiwa Dental Clinic. He can be reached by contacting Dr. Samuel Kratchman at sikratch@comcast.net.
Dr. Kratsman he received his BA in Biology and DMD from Tufts University in Boston and his Endodontics certificate from the University of Pennsylvania, where he is Associate Professor of Endodontics, Assistant Director of Graduate Endodontics and Chief of Microsurgery. Dr. Kratchman co-authored the manual Microsurgery in Endodontics with Dr. Syngcuk Kim in 2017 and developed a patented instrument called the S-Kondenser to unclog root canals. Dr. Kratchman lectures nationally and internationally in addition to maintaining 4 private practices in Exton, West Chester, Paoli and Bryn Mawr, Pa. He can be reached at sikratch@comcast.net.
Disclosure: The authors report no disclosures.


